Back

Poster Session E - Tuesday Afternoon
Category: Biliary/Pancreas
E0018 - Disparities in the Readmission Rates After Hospitalization for Acute Pancreatitis
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Muhammad Sheharyar Warraich, MD, MBBS
John H. Stroger Jr. Hospital of Cook County
Chicago, IL
Presenting Author(s)
Muhammad Sheharyar Warraich, MD, MBBS1, Dae Y. Park, MD2, Michelle Ishaya, DO2, Katayoun Khoshbin, MD2, Jawad Ahmed, MBBS3, Bashar Attar, MD2
1John H. Stroger Jr. Hospital of Cook County, Chicago, IL; 2John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 3Dow University of Health Sciences, Karachi, Sindh, Pakistan
Introduction: Acute pancreatitis (AP) is one of the leading causes of hospitalization in the United States. Patients with AP frequently get readmitted and that proves to be a great burden on our healthcare system. Age, male sex, tobacco use, alcohol use, and necrotizing pancreatitis have been linked to a higher readmission rate in AP patients. However, studies on the impact of socioeconomic status are lacking. Our study attempts to find the impact of income on the readmission rates in patients admitted for AP.
Methods: We queried the National Readmission Database (NRD) from 2017 to 2018 to identify patients with a primary diagnosis of AP. Those who died during the index hospitalization were excluded when examining readmission rates. Multivariable Cox proportional-hazards regression was used to study the impact of income on 90-day readmission adjusted for age, sex, comorbidities, hospital characteristics, and primary payer.
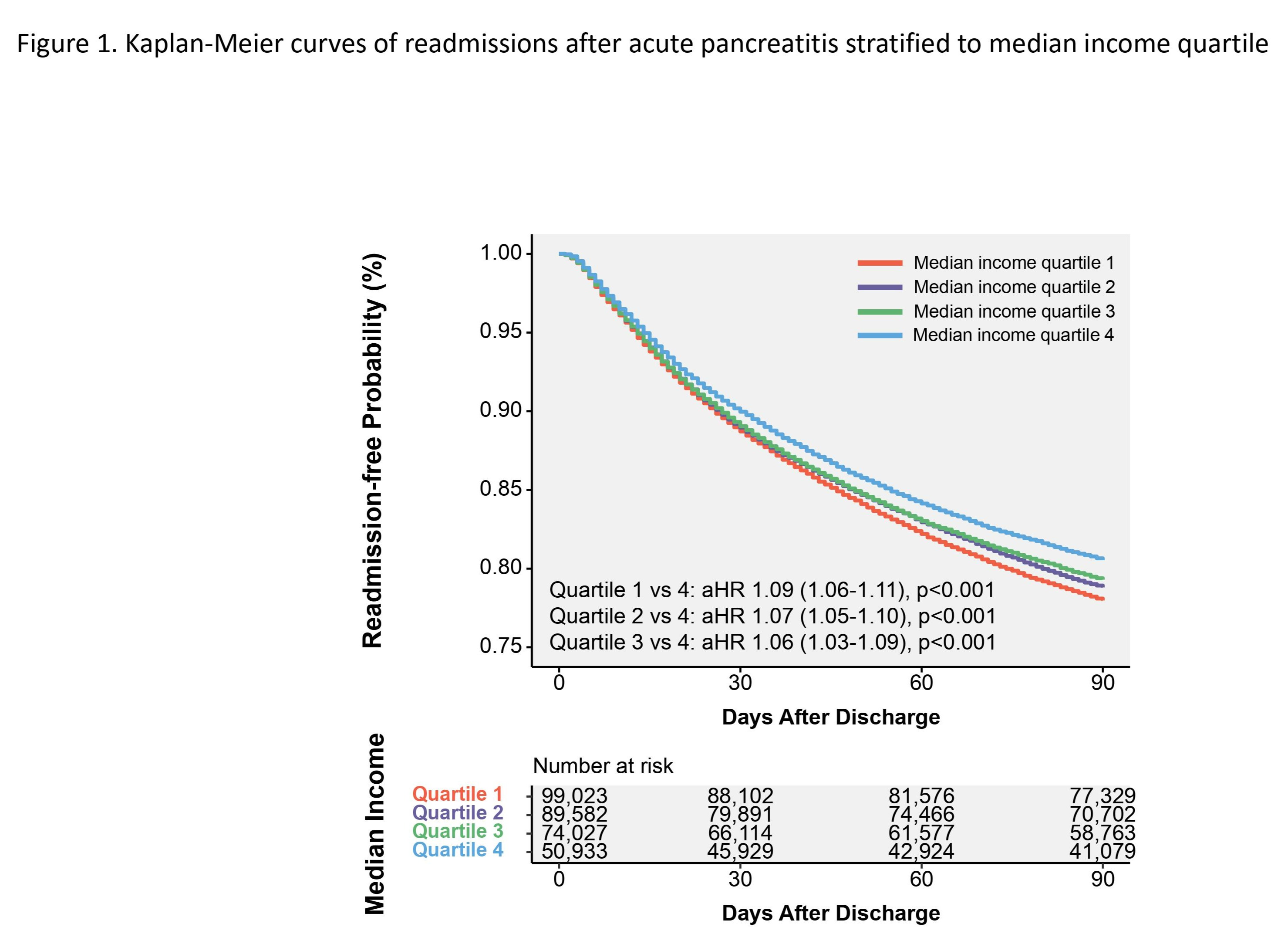
Results: A total of 313,565 AP patients were identified, 99,023 of whom belonged to median income quartile 1, 89,582 to quartile 2, 74,027 to quartile 3, and 50,933 to quartile 4 with quartile 4 having the highest income. Slightly more than half of each quartile group were men (53.1%, 52.8%, 53.0%, 53.5%, respectively). Patients with lower income had higher prevalence of comorbidities. Among those who survived the index hospitalization, 21,694 (21.9%), 18,880 (21.1%), 15,264 (20.6%), and 9,854 (19.3%) patients in quartiles 1, 2, 3, and 4 were readmitted within 90 days, respectively. When compared with the highest income quartile (quartile 4), patients in quartiles 1, 2, and 3 were associated with an increasingly higher hazard of readmission (quartile 1, aHR 1.09, p< 0.001; quartile 2, aHR 1.07, p< 0.001; quartile 3, aHR 1.06, p< 0.001).
Discussion: Our study finds a positive correlation between poverty and the 90-day readmission rate in AP patients. Alcohol use is one of the top causes of pancreatitis in the US. It would be interesting to investigate if there is a difference in the prevalence of substance use in patients of various economic strata that could be impacting the readmission. Furthermore, it is imperative that we bring reforms in our financial and health policy to make it more equitable in order to alleviate some of the disparities we see.
Disclosures:
Muhammad Sheharyar Warraich, MD, MBBS1, Dae Y. Park, MD2, Michelle Ishaya, DO2, Katayoun Khoshbin, MD2, Jawad Ahmed, MBBS3, Bashar Attar, MD2. E0018 - Disparities in the Readmission Rates After Hospitalization for Acute Pancreatitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1John H. Stroger Jr. Hospital of Cook County, Chicago, IL; 2John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 3Dow University of Health Sciences, Karachi, Sindh, Pakistan
Introduction: Acute pancreatitis (AP) is one of the leading causes of hospitalization in the United States. Patients with AP frequently get readmitted and that proves to be a great burden on our healthcare system. Age, male sex, tobacco use, alcohol use, and necrotizing pancreatitis have been linked to a higher readmission rate in AP patients. However, studies on the impact of socioeconomic status are lacking. Our study attempts to find the impact of income on the readmission rates in patients admitted for AP.
Methods: We queried the National Readmission Database (NRD) from 2017 to 2018 to identify patients with a primary diagnosis of AP. Those who died during the index hospitalization were excluded when examining readmission rates. Multivariable Cox proportional-hazards regression was used to study the impact of income on 90-day readmission adjusted for age, sex, comorbidities, hospital characteristics, and primary payer.
Results: A total of 313,565 AP patients were identified, 99,023 of whom belonged to median income quartile 1, 89,582 to quartile 2, 74,027 to quartile 3, and 50,933 to quartile 4 with quartile 4 having the highest income. Slightly more than half of each quartile group were men (53.1%, 52.8%, 53.0%, 53.5%, respectively). Patients with lower income had higher prevalence of comorbidities. Among those who survived the index hospitalization, 21,694 (21.9%), 18,880 (21.1%), 15,264 (20.6%), and 9,854 (19.3%) patients in quartiles 1, 2, 3, and 4 were readmitted within 90 days, respectively. When compared with the highest income quartile (quartile 4), patients in quartiles 1, 2, and 3 were associated with an increasingly higher hazard of readmission (quartile 1, aHR 1.09, p< 0.001; quartile 2, aHR 1.07, p< 0.001; quartile 3, aHR 1.06, p< 0.001).
Discussion: Our study finds a positive correlation between poverty and the 90-day readmission rate in AP patients. Alcohol use is one of the top causes of pancreatitis in the US. It would be interesting to investigate if there is a difference in the prevalence of substance use in patients of various economic strata that could be impacting the readmission. Furthermore, it is imperative that we bring reforms in our financial and health policy to make it more equitable in order to alleviate some of the disparities we see.
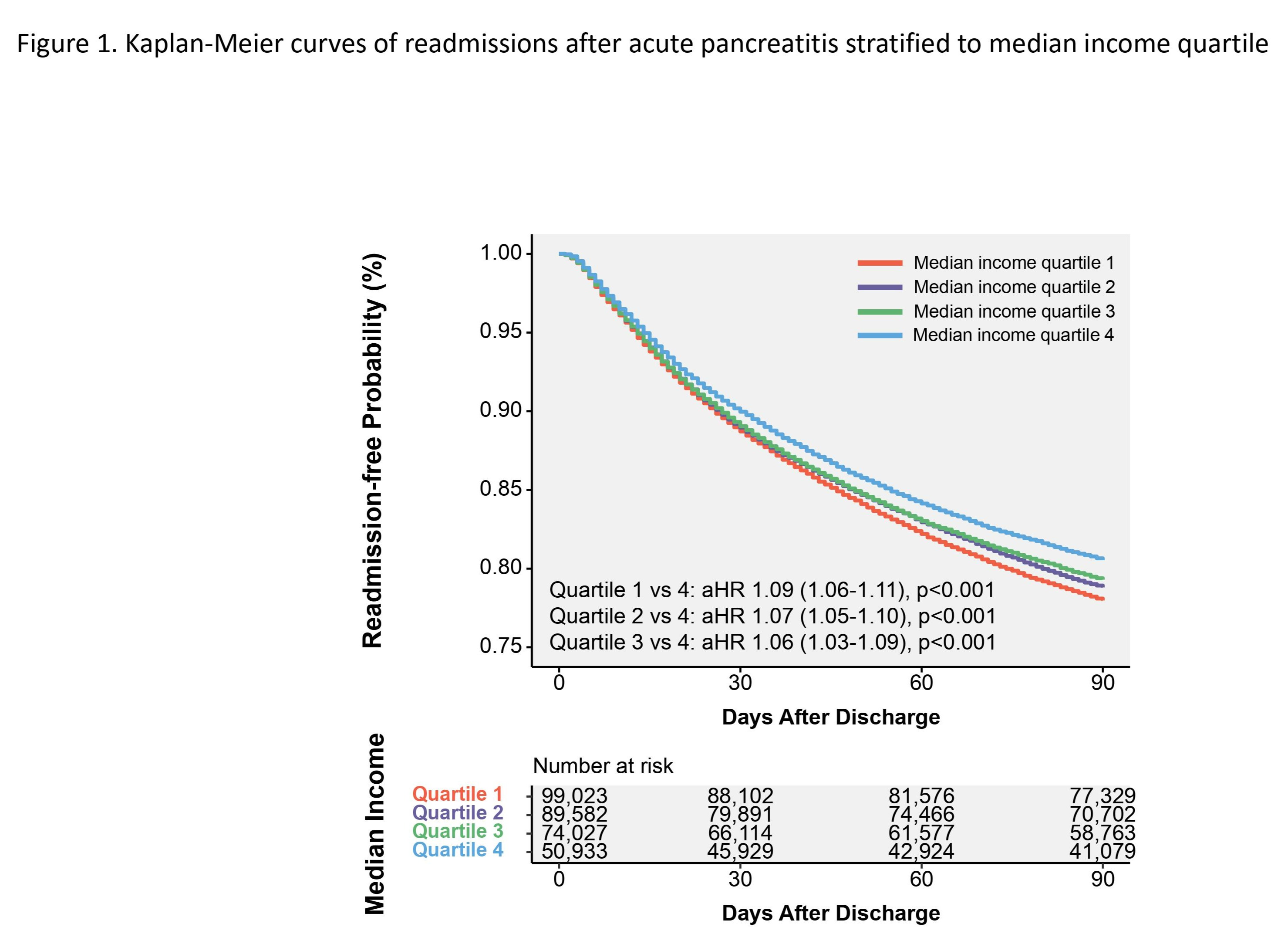
Figure: Kaplan-Meier curves of readmissions after acute pancreatitis stratified to median income quartile
Disclosures:
Muhammad Sheharyar Warraich indicated no relevant financial relationships.
Dae Park indicated no relevant financial relationships.
Michelle Ishaya indicated no relevant financial relationships.
Katayoun Khoshbin indicated no relevant financial relationships.
Jawad Ahmed indicated no relevant financial relationships.
Bashar Attar indicated no relevant financial relationships.
Muhammad Sheharyar Warraich, MD, MBBS1, Dae Y. Park, MD2, Michelle Ishaya, DO2, Katayoun Khoshbin, MD2, Jawad Ahmed, MBBS3, Bashar Attar, MD2. E0018 - Disparities in the Readmission Rates After Hospitalization for Acute Pancreatitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
