Back
Poster Session E - Tuesday Afternoon
Category: Biliary/Pancreas
E0044 - Recurrent Shock in a 31-Year-Old Woman With Chronic Pancreatitis and Cirrhosis
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Bradley Busebee, MD
Mayo Clinic
Rochester, MN
Presenting Author(s)
Bradley Busebee, MD1, Lea N. Sayegh, MD2, Benjamin R. Stultz, MD1, Ahmed T. Kurdi, MD1, Nayantara Coelho Prabhu, MD1
1Mayo Clinic, Rochester, MN; 2American University of Beirut, Beirut, Beyrouth, Lebanon
Introduction: Below is the case of a 31 year old woman with recurrent shock in the setting of chronic pancreatitis and cirrhosis.
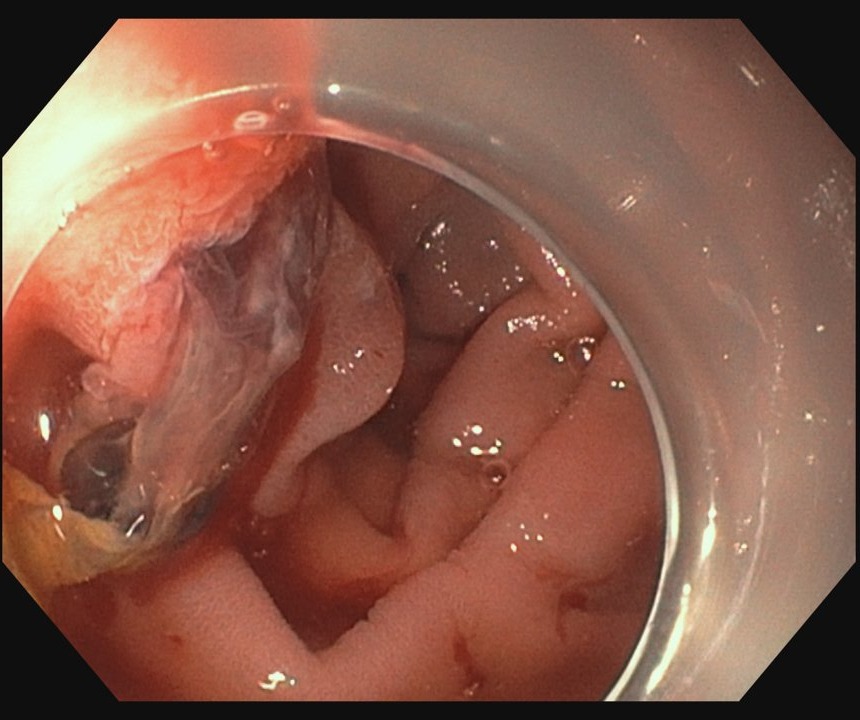
Case Description/Methods: A 31-year-old woman with decompensated alcoholic cirrhosis and chronic pancreatitis presented with shock in the setting of epistaxis and tertiary adrenal insufficiency. Endoscopy was initially deferred as evaluation a month prior upon similar presentation with epistaxis and hematochezia showed no luminal evidence or sources of bleeding. During her repeat admission, she required pressor support and stress dose steroids with spontaneous cessation of epistaxis and resolution of shock. She subsequently developed hematochezia. Repeat EGD demonstrated fresh blood and clots emancipating from the ampulla. CT angiography revealed active arterial bleeding within the pancreatic head, consistent with hemosuccus pancreaticus (HP), as well as acute on chronic pancreatitis with peripancreatic fluid collections in the head and tail. Hemostasis was achieved via IR guided coil embolization of the right gastroepiploic artery and gel foam embolization of the gastroduodenal artery and pancreaticoduodenal arcade.
Discussion: HP is a rare cause of gastrointestinal hemorrhage which describes bleeding from the duodenal papilla via the pancreatic duct. The intermittent nature of the bleeding likely explains the frequency of negative endoscopy and delays in diagnosis. Endovascular and surgical management are effective in controlling hemorrhage and reducing mortality, which may exceed 90% without adequate intervention. Chronic pancreatitis is present in 76% of cases of HP and acute pancreatitis is present in 13%. Other, rare etiologies of HP include neoplasm and trauma. Pancreatitis induced inflammation and erosion likely promote vessel degradation and pseudoaneurysm formation. Pseudoaneurysm rupture is the most common cause of HP and as many as 98% of patients with HP have >1 pseudoaneurysm. A minority of patients with HP have no identifiable pseudoaneurysm. The case herein is notable for a number of atypical features, including the infrequent co-occurrence of alcohol induced cirrhosis and pancreatitis with such an early age of onset, as well as involvement of atypical vasculature. The case underscores the importance of a low threshold for repeat endoscopic evaluation of hemorrhagic shock, particularly in patients with high-risk comorbidities.
Disclosures:
Bradley Busebee, MD1, Lea N. Sayegh, MD2, Benjamin R. Stultz, MD1, Ahmed T. Kurdi, MD1, Nayantara Coelho Prabhu, MD1. E0044 - Recurrent Shock in a 31-Year-Old Woman With Chronic Pancreatitis and Cirrhosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Mayo Clinic, Rochester, MN; 2American University of Beirut, Beirut, Beyrouth, Lebanon
Introduction: Below is the case of a 31 year old woman with recurrent shock in the setting of chronic pancreatitis and cirrhosis.
Case Description/Methods: A 31-year-old woman with decompensated alcoholic cirrhosis and chronic pancreatitis presented with shock in the setting of epistaxis and tertiary adrenal insufficiency. Endoscopy was initially deferred as evaluation a month prior upon similar presentation with epistaxis and hematochezia showed no luminal evidence or sources of bleeding. During her repeat admission, she required pressor support and stress dose steroids with spontaneous cessation of epistaxis and resolution of shock. She subsequently developed hematochezia. Repeat EGD demonstrated fresh blood and clots emancipating from the ampulla. CT angiography revealed active arterial bleeding within the pancreatic head, consistent with hemosuccus pancreaticus (HP), as well as acute on chronic pancreatitis with peripancreatic fluid collections in the head and tail. Hemostasis was achieved via IR guided coil embolization of the right gastroepiploic artery and gel foam embolization of the gastroduodenal artery and pancreaticoduodenal arcade.
Discussion: HP is a rare cause of gastrointestinal hemorrhage which describes bleeding from the duodenal papilla via the pancreatic duct. The intermittent nature of the bleeding likely explains the frequency of negative endoscopy and delays in diagnosis. Endovascular and surgical management are effective in controlling hemorrhage and reducing mortality, which may exceed 90% without adequate intervention. Chronic pancreatitis is present in 76% of cases of HP and acute pancreatitis is present in 13%. Other, rare etiologies of HP include neoplasm and trauma. Pancreatitis induced inflammation and erosion likely promote vessel degradation and pseudoaneurysm formation. Pseudoaneurysm rupture is the most common cause of HP and as many as 98% of patients with HP have >1 pseudoaneurysm. A minority of patients with HP have no identifiable pseudoaneurysm. The case herein is notable for a number of atypical features, including the infrequent co-occurrence of alcohol induced cirrhosis and pancreatitis with such an early age of onset, as well as involvement of atypical vasculature. The case underscores the importance of a low threshold for repeat endoscopic evaluation of hemorrhagic shock, particularly in patients with high-risk comorbidities.
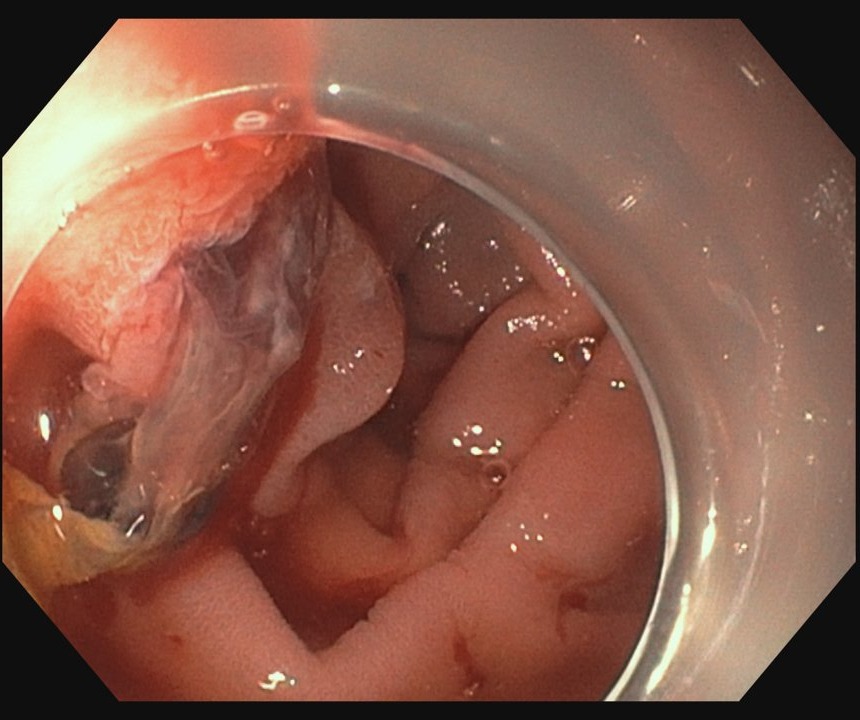
Figure: Fresh blood and clots protruding for the ampulla
Disclosures:
Bradley Busebee indicated no relevant financial relationships.
Lea Sayegh indicated no relevant financial relationships.
Benjamin Stultz indicated no relevant financial relationships.
Ahmed Kurdi indicated no relevant financial relationships.
Nayantara Coelho Prabhu indicated no relevant financial relationships.
Bradley Busebee, MD1, Lea N. Sayegh, MD2, Benjamin R. Stultz, MD1, Ahmed T. Kurdi, MD1, Nayantara Coelho Prabhu, MD1. E0044 - Recurrent Shock in a 31-Year-Old Woman With Chronic Pancreatitis and Cirrhosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
