Back


Poster Session B - Monday Morning
Category: Esophagus
B0251 - Endoscopic Balloon Dilation of Recurrent Peptic Stricture in a Patient With Portal Hypertension
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom

Has Audio

Fadi Chanaa, MD
Atrium Health Wake Forest Baptist Medical Center
Winston-Salem, North Carolina
Presenting Author(s)
Fadi Chanaa, MD1, Steven Clayton, MD2
1Atrium Health Wake Forest Baptist Medical Center, Winston-Salem, NC; 2Wake Forest Baptist Medical Center, Winston-Salem, NC
Introduction: Variceal hemorrhage is a devastating complication and a major cause of mortality in patients with portal hypertension. Unfortunately, one third of patients with varices develop bleeding in their lifetime. This case depicts a rarely reported intervention that physicians may be hesitant to pursue.
Case Description/Methods: A 61 year old male with history significant for atrial fibrillation (afib), alcoholic cirrhosis complicated by gastric and esophageal varices, and GERD presented with dysphagia. He previously underwent endoscopic variceal band ligation (EVL) in 2009 for primary prevention of esophageal varices and placed on daily nadolol. His GERD was controlled with twice daily PPI and as-needed H2 antagonist. Despite this, he developed strictures secondary to severe erosive esophagitis. He was then started on apixaban for afib and transitioned from nadolol to carvedilol. His MELD-Na is 8 and had a reported distant history of hepatic encephalopathy.
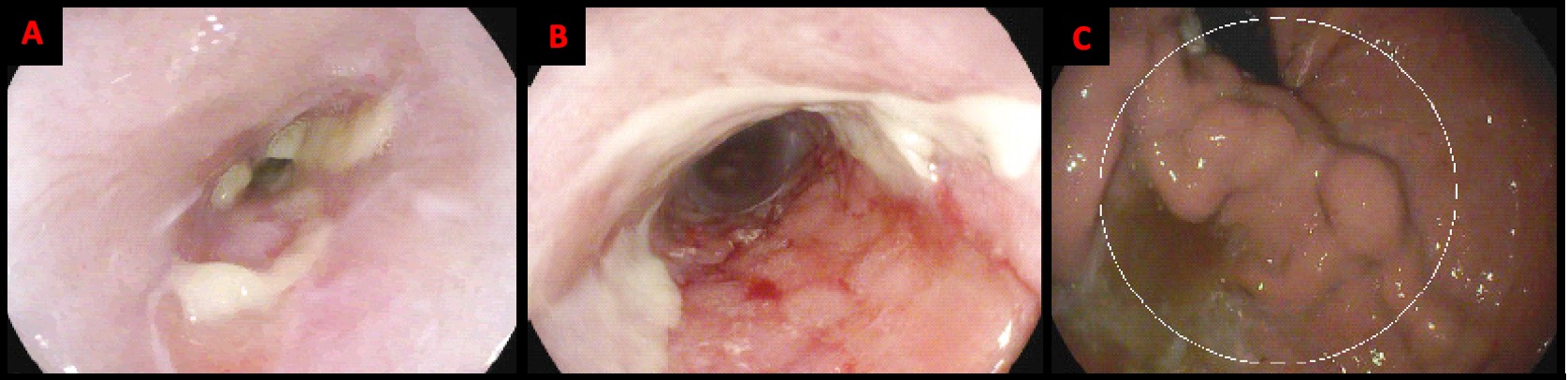
He presented to the esophageal motility clinic with progressive dysphagia to both solids and liquids. An EGD was scheduled which revealed a partially obstructive ulcerative stricture spanning 29 - 34 cm from incisors. The stricture was injected with 4 ml of triamcinolone acetonide distributed in 1 cm increments across four quadrants. Then the stricture was dilated with a 10-12 mm cre balloon under fluoroscopic guidance. Dilation caused shallow mucosal tears with scant blood but otherwise no significant bleeding or complication. The scope was traversed into the stomach with retroflexion revealing moderate gastric varices in the cardia. After the procedure was completed, the patient had complete resolvent of symptoms and tolerated oral nutrition.
Discussion: This case describes a cirrhotic patient with portal hypertension requiring frequent endoscopic balloon dilations for severe dysphagia secondary to recurrent peptic strictures. Extensive literature review did not reveal any documented cases describing this scenario. The presence of gastric varices in this patient is indicative of active portal hypertension. This in combination with the patient’s anticoagulation places a theoretical high risk of bleeding during the procedure. Although this case demonstrates that it is safe to perform serial dilations in patients with portal hypertension if they have undergone EVL and do not have active esophageal varices.
Disclosures:
Fadi Chanaa, MD1, Steven Clayton, MD2. B0251 - Endoscopic Balloon Dilation of Recurrent Peptic Stricture in a Patient With Portal Hypertension, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Atrium Health Wake Forest Baptist Medical Center, Winston-Salem, NC; 2Wake Forest Baptist Medical Center, Winston-Salem, NC
Introduction: Variceal hemorrhage is a devastating complication and a major cause of mortality in patients with portal hypertension. Unfortunately, one third of patients with varices develop bleeding in their lifetime. This case depicts a rarely reported intervention that physicians may be hesitant to pursue.
Case Description/Methods: A 61 year old male with history significant for atrial fibrillation (afib), alcoholic cirrhosis complicated by gastric and esophageal varices, and GERD presented with dysphagia. He previously underwent endoscopic variceal band ligation (EVL) in 2009 for primary prevention of esophageal varices and placed on daily nadolol. His GERD was controlled with twice daily PPI and as-needed H2 antagonist. Despite this, he developed strictures secondary to severe erosive esophagitis. He was then started on apixaban for afib and transitioned from nadolol to carvedilol. His MELD-Na is 8 and had a reported distant history of hepatic encephalopathy.
He presented to the esophageal motility clinic with progressive dysphagia to both solids and liquids. An EGD was scheduled which revealed a partially obstructive ulcerative stricture spanning 29 - 34 cm from incisors. The stricture was injected with 4 ml of triamcinolone acetonide distributed in 1 cm increments across four quadrants. Then the stricture was dilated with a 10-12 mm cre balloon under fluoroscopic guidance. Dilation caused shallow mucosal tears with scant blood but otherwise no significant bleeding or complication. The scope was traversed into the stomach with retroflexion revealing moderate gastric varices in the cardia. After the procedure was completed, the patient had complete resolvent of symptoms and tolerated oral nutrition.
Discussion: This case describes a cirrhotic patient with portal hypertension requiring frequent endoscopic balloon dilations for severe dysphagia secondary to recurrent peptic strictures. Extensive literature review did not reveal any documented cases describing this scenario. The presence of gastric varices in this patient is indicative of active portal hypertension. This in combination with the patient’s anticoagulation places a theoretical high risk of bleeding during the procedure. Although this case demonstrates that it is safe to perform serial dilations in patients with portal hypertension if they have undergone EVL and do not have active esophageal varices.
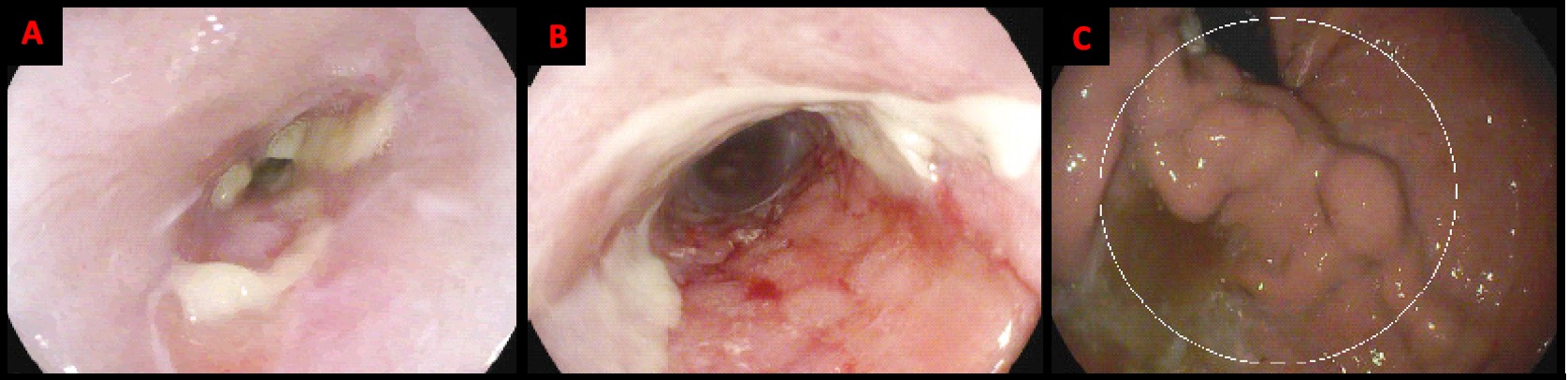
Figure: A) EGD showed ulcerative peptic stricture located in the mid-esophagus. (B) There was scant bleeding after dilation, otherwise no significant bleeding or complication. (C) Retroflexion was performed in the stomach and revealed moderate gastric varies in the cardia.
Disclosures:
Fadi Chanaa indicated no relevant financial relationships.
Steven Clayton indicated no relevant financial relationships.
Fadi Chanaa, MD1, Steven Clayton, MD2. B0251 - Endoscopic Balloon Dilation of Recurrent Peptic Stricture in a Patient With Portal Hypertension, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

