Back
Poster Session B - Monday Morning
Category: Liver
B0617 - A Case of Seronegative Autoimmune Hepatitis During Pregnancy
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
- SG
Sanda Gomez-Paz, MD
Nassau University Medical Center
East Meadow, NY
Presenting Author(s)
Sandra Gomez-Paz, MD, Kevin Yeroushalmi, MD, Jiten Desai, MD, Rajmohan Rammohan, MD, Deepthi Kagolanu, MD, Kaleem Rizvon, , Nausheer Khan, MD, Paul Mustacchia, MD, MBA
Nassau University Medical Center, East Meadow, NY
Introduction: Autoimmune hepatitis (AIH) is a rare disease that usually affects women at reproductive age and is associated with an increased risk of adverse maternal and fetal outcomes. Diagnosis of AIH during pregnancy, particularly in absence of autoantibodies, poses a challenge for clinicians. We present the case of a patient with new-onset seronegative AIH during pregnancy.
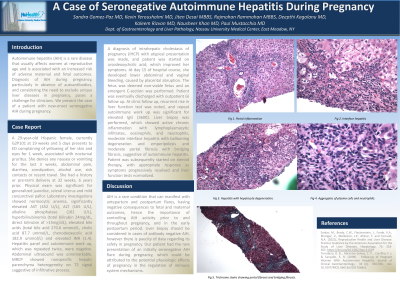
Case Description/Methods: A 29-year-old Hispanic female, G2P101 at 19 weeks presents complaining of yellowing of her skin and eyes for 1 week, associated with nocturnal pruritus. Physical exam showed generalized jaundice and scleral icterus. Laboratory investigations showed significantly elevated AST (452 U/L), ALT (165 U/L), alkaline phosphatase (182 U/L), hyperbilirubinemia, elevated bile acids, and elevated INR. Hepatitis panel and autoimmune work up, were negative. Abdominal ultrasound was normal. MRCP showed nonspecific hepatic parenchyma heterogeneity on T2 signal suggestive of infiltrative process. A diagnosis of intrahepatic cholestasis of pregnancy (IHCP) with atypical presentation was made, and patient was started on ursodeoxycholic acid, which improved her symptoms. At day 15, she developed lower abdominal and vaginal bleeding, caused by placental abruption. The fetus was deemed non-viable and an emergent C-section was performed. Patient was eventually discharged with outpatient GI follow up. At follow up, recurrent rise in liver function tests were noted, and repeat autoimmune work up showed elevated IgG (3600). Liver biopsy was performed, which showed active chronic inflammation with lymphoplasmacytic infiltrates, moderate interface hepatitis with ballooning degeneration and emperipolesis, and moderate portal fibrosis with bridging fibrosis, suggestive of autoimmune hepatitis. Patient was subsequently started on steroid therapy, with appropriate response as symptoms progressively resolved and liver function tests normalized.
Discussion: AIH is a rare condition that can manifest with antepartum and postpartum flares, having negative consequences to fetal and maternal outcomes, hence the importance of controlling AIH activity throughout pregnancy and in the postpartum period. Liver biopsy should be considered in cases of antibody negative AIH, however there is paucity of data regarding its safety in pregnancy. We present the rare case of an initially seronegative AIH flare during pregnancy, possibly attributed to the potential physiologic effects of pregnancy in the regulation of immune system mechanisms.
Disclosures:
Sandra Gomez-Paz, MD, Kevin Yeroushalmi, MD, Jiten Desai, MD, Rajmohan Rammohan, MD, Deepthi Kagolanu, MD, Kaleem Rizvon, , Nausheer Khan, MD, Paul Mustacchia, MD, MBA. B0617 - A Case of Seronegative Autoimmune Hepatitis During Pregnancy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Nassau University Medical Center, East Meadow, NY
Introduction: Autoimmune hepatitis (AIH) is a rare disease that usually affects women at reproductive age and is associated with an increased risk of adverse maternal and fetal outcomes. Diagnosis of AIH during pregnancy, particularly in absence of autoantibodies, poses a challenge for clinicians. We present the case of a patient with new-onset seronegative AIH during pregnancy.
Case Description/Methods: A 29-year-old Hispanic female, G2P101 at 19 weeks presents complaining of yellowing of her skin and eyes for 1 week, associated with nocturnal pruritus. Physical exam showed generalized jaundice and scleral icterus. Laboratory investigations showed significantly elevated AST (452 U/L), ALT (165 U/L), alkaline phosphatase (182 U/L), hyperbilirubinemia, elevated bile acids, and elevated INR. Hepatitis panel and autoimmune work up, were negative. Abdominal ultrasound was normal. MRCP showed nonspecific hepatic parenchyma heterogeneity on T2 signal suggestive of infiltrative process. A diagnosis of intrahepatic cholestasis of pregnancy (IHCP) with atypical presentation was made, and patient was started on ursodeoxycholic acid, which improved her symptoms. At day 15, she developed lower abdominal and vaginal bleeding, caused by placental abruption. The fetus was deemed non-viable and an emergent C-section was performed. Patient was eventually discharged with outpatient GI follow up. At follow up, recurrent rise in liver function tests were noted, and repeat autoimmune work up showed elevated IgG (3600). Liver biopsy was performed, which showed active chronic inflammation with lymphoplasmacytic infiltrates, moderate interface hepatitis with ballooning degeneration and emperipolesis, and moderate portal fibrosis with bridging fibrosis, suggestive of autoimmune hepatitis. Patient was subsequently started on steroid therapy, with appropriate response as symptoms progressively resolved and liver function tests normalized.
Discussion: AIH is a rare condition that can manifest with antepartum and postpartum flares, having negative consequences to fetal and maternal outcomes, hence the importance of controlling AIH activity throughout pregnancy and in the postpartum period. Liver biopsy should be considered in cases of antibody negative AIH, however there is paucity of data regarding its safety in pregnancy. We present the rare case of an initially seronegative AIH flare during pregnancy, possibly attributed to the potential physiologic effects of pregnancy in the regulation of immune system mechanisms.
Disclosures:
Sandra Gomez-Paz indicated no relevant financial relationships.
Kevin Yeroushalmi indicated no relevant financial relationships.
Jiten Desai indicated no relevant financial relationships.
Rajmohan Rammohan indicated no relevant financial relationships.
Deepthi Kagolanu indicated no relevant financial relationships.
Kaleem Rizvon indicated no relevant financial relationships.
Nausheer Khan indicated no relevant financial relationships.
Paul Mustacchia indicated no relevant financial relationships.
Sandra Gomez-Paz, MD, Kevin Yeroushalmi, MD, Jiten Desai, MD, Rajmohan Rammohan, MD, Deepthi Kagolanu, MD, Kaleem Rizvon, , Nausheer Khan, MD, Paul Mustacchia, MD, MBA. B0617 - A Case of Seronegative Autoimmune Hepatitis During Pregnancy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
