Back

Poster Session B - Monday Morning
Category: Interventional Endoscopy
B0466 - Weight Loss Utilizing Endoscopic Sleeve Gastroplasty (ESG), Benefit for Ostomy Reversal in Obese Patient With Ulcerative Colitis (UC)
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- AC
Abhishek A. Chouthai, MD
Cooper Medical School at Rowan University, Cooper University Hospital
New Brunswick, NJ
Presenting Author(s)
Abhishek A. Chouthai, MD1, Mihajlo Gjeorgjievski, MD2, Avik Sarkar, MD2
1Cooper Medical School at Rowan University, Cooper University Hospital, New Brunswick, NJ; 2Robert Wood Johnson Medical School, Rutgers University, New Brunswick, NJ
Introduction: Over the last thirty years, the prevalence of both obesity and inflammatory bowel disease has increased globally. Surgical management in ulcerative colitis (UC) is reserved for medically refractory UC, most typically in a three-stage pattern: initial removal of the colon and creation of an end ileostomy, followed by removal of the rectum and construction of ileal pouch anal anastomosis and diverting ileostomy, followed by reversal of the ileostomy. Proctectomy is particularly difficult in obese patients due to increased visceral adiposity, thickened abdominal wall, adhesions, and reduced mobility secondary to bulky mesentery. Patients with Body Mass Index (BMI) greater than 30 are found to have greater risk for complications in comparison to normal BMI counterparts. Endoscopic sleeve gastroplasty (ESG) is a newer, minimally invasive procedure for the treatment of obesity which endoscopically reduces gastric volume through an endoscopic suturing system. We present a novel case where ESG was used as a tool for weight loss in a patient who encountered delayed ostomy reversal due to morbid obesity.
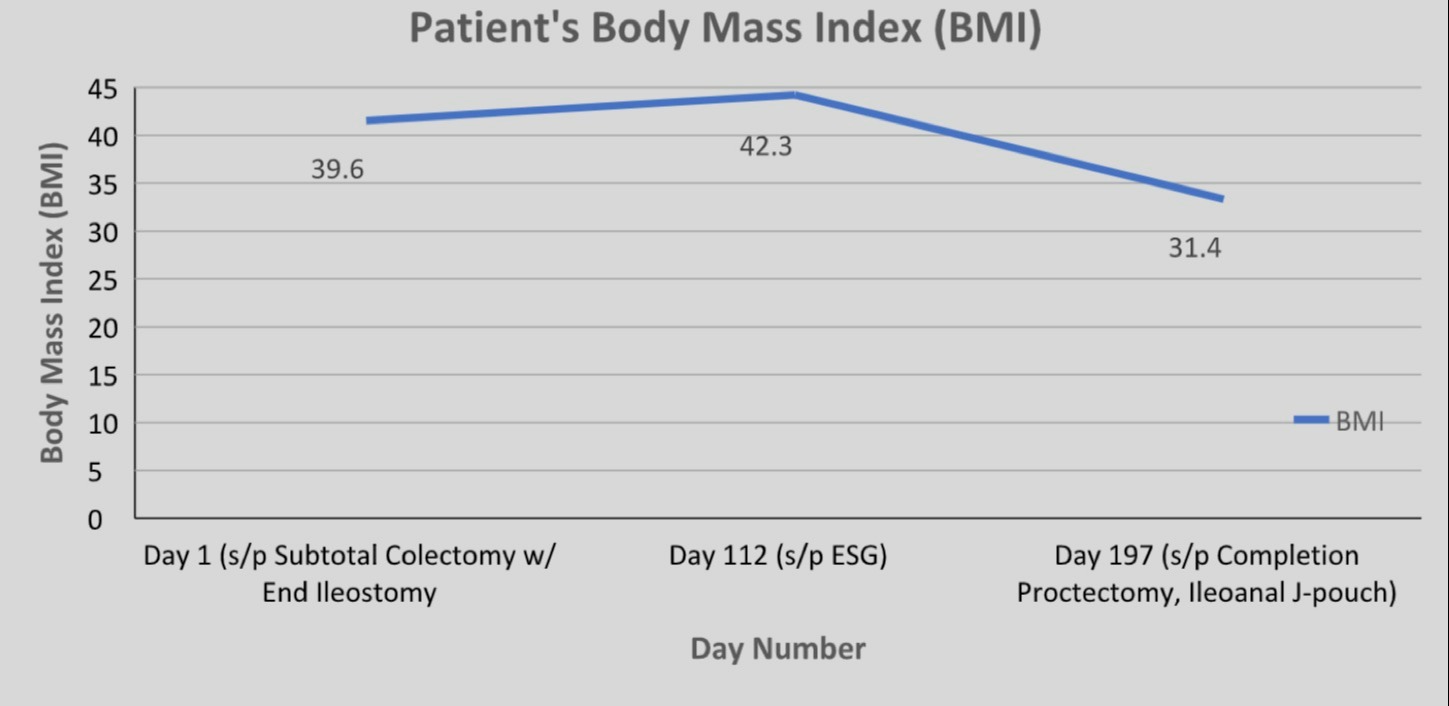
Case Description/Methods: A 39-year-old man with medical history significant for morbid obesity and medically refractory UC became a candidate for proctocolectomy with an ileal pouch anal anastomosis. However, given the patient’s obesity, there was concern of the J-pouch-end ileostomy being unable to reach the patient’s pelvis. Patient underwent a da Vinci assisted laparoscopic subtotal colectomy with end ileostomy in order to preserve the rectum for a potential J-pouch after his weight loss. Post subtotal colectomy and end ileostomy, patient was referred for endoscopic sleeve gastroplasty due to additional weight gain post-op due to symptom mediated inactivity, thereby further delaying his ostomy reversal and placement of ileoanal J-pouch. Patient underwent endoscopic sleeve gastrectomy (ESG) with effective weight loss, anatomically allowing successful ostomy reversal, completion proctectomy, and J-tube construction.
Discussion: Future studies are required to determine whether ESG weight loss should be an integral initial step of medical management of IBD in obese patients to inevitably avoid surgical intervention. In summary, ESG may be a pivotal modality as a tool for weight loss in patients with UC and morbid obesity who may encounter delayed proctectomy and ostomy reversal, overall helping contribute to decreased surgical morbidity, complications, and faster improvement in overall quality of life.
Disclosures:
Abhishek A. Chouthai, MD1, Mihajlo Gjeorgjievski, MD2, Avik Sarkar, MD2. B0466 - Weight Loss Utilizing Endoscopic Sleeve Gastroplasty (ESG), Benefit for Ostomy Reversal in Obese Patient With Ulcerative Colitis (UC), ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Cooper Medical School at Rowan University, Cooper University Hospital, New Brunswick, NJ; 2Robert Wood Johnson Medical School, Rutgers University, New Brunswick, NJ
Introduction: Over the last thirty years, the prevalence of both obesity and inflammatory bowel disease has increased globally. Surgical management in ulcerative colitis (UC) is reserved for medically refractory UC, most typically in a three-stage pattern: initial removal of the colon and creation of an end ileostomy, followed by removal of the rectum and construction of ileal pouch anal anastomosis and diverting ileostomy, followed by reversal of the ileostomy. Proctectomy is particularly difficult in obese patients due to increased visceral adiposity, thickened abdominal wall, adhesions, and reduced mobility secondary to bulky mesentery. Patients with Body Mass Index (BMI) greater than 30 are found to have greater risk for complications in comparison to normal BMI counterparts. Endoscopic sleeve gastroplasty (ESG) is a newer, minimally invasive procedure for the treatment of obesity which endoscopically reduces gastric volume through an endoscopic suturing system. We present a novel case where ESG was used as a tool for weight loss in a patient who encountered delayed ostomy reversal due to morbid obesity.
Case Description/Methods: A 39-year-old man with medical history significant for morbid obesity and medically refractory UC became a candidate for proctocolectomy with an ileal pouch anal anastomosis. However, given the patient’s obesity, there was concern of the J-pouch-end ileostomy being unable to reach the patient’s pelvis. Patient underwent a da Vinci assisted laparoscopic subtotal colectomy with end ileostomy in order to preserve the rectum for a potential J-pouch after his weight loss. Post subtotal colectomy and end ileostomy, patient was referred for endoscopic sleeve gastroplasty due to additional weight gain post-op due to symptom mediated inactivity, thereby further delaying his ostomy reversal and placement of ileoanal J-pouch. Patient underwent endoscopic sleeve gastrectomy (ESG) with effective weight loss, anatomically allowing successful ostomy reversal, completion proctectomy, and J-tube construction.
Discussion: Future studies are required to determine whether ESG weight loss should be an integral initial step of medical management of IBD in obese patients to inevitably avoid surgical intervention. In summary, ESG may be a pivotal modality as a tool for weight loss in patients with UC and morbid obesity who may encounter delayed proctectomy and ostomy reversal, overall helping contribute to decreased surgical morbidity, complications, and faster improvement in overall quality of life.
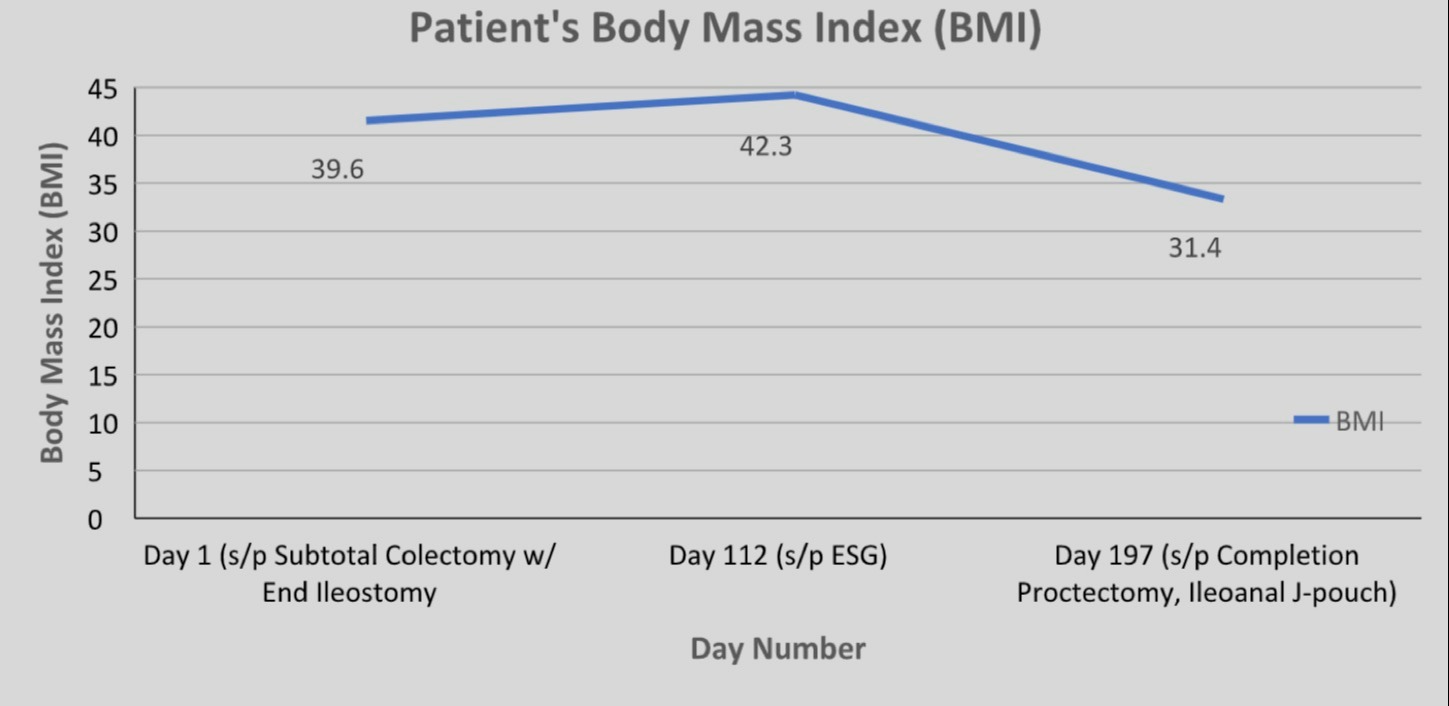
Figure: Clinical management and BMI over patient's clinical course.
Disclosures:
Abhishek Chouthai indicated no relevant financial relationships.
Mihajlo Gjeorgjievski indicated no relevant financial relationships.
Avik Sarkar indicated no relevant financial relationships.
Abhishek A. Chouthai, MD1, Mihajlo Gjeorgjievski, MD2, Avik Sarkar, MD2. B0466 - Weight Loss Utilizing Endoscopic Sleeve Gastroplasty (ESG), Benefit for Ostomy Reversal in Obese Patient With Ulcerative Colitis (UC), ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
