Back
Poster Session E - Tuesday Afternoon
Category: Biliary/Pancreas
E0057 - Portal Biliopathy in a Patient Who Underwent a Whipple Procedure With Portal Vein Reconstruction
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Michael J. Mintz, MD
New York-Presbyterian Hospital/Weill Cornell Medicine
New York, New York
Presenting Author(s)
Zuhair Sadiq, BA1, Khalifa Bshesh, BA1, Michael J. Mintz, MD2, Malorie Simons, MD2, Allison Yang, MD3
1Weill Cornell Medical College, New York, NY; 2New York-Presbyterian Hospital/Weill Cornell Medicine, New York, NY; 3New York Presbyterian Hospital/ Weill Cornell Medicine, New York, NY
Introduction: Portal biliopathy is a condition that is defined as abnormalities in the biliary tract due to portal hypertension. Some patients may present with abdominal pain, fever, jaundice, or pruritis. Rarely, portal hypertension secondary to portal vein abnormalities cause peri-biliary varices. We report a case of a patient with a peri-biliary variceal bleed due to portal hypertension from acquired portal vein stenosis.
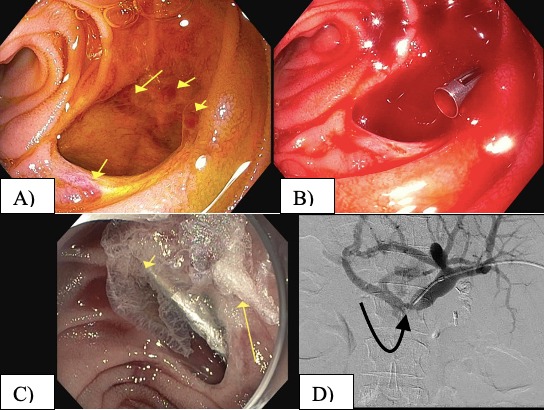
Case Description/Methods: A 59-year-old female with a past medical history of pancreatic ductal adenocarcinoma presented to the hospital with 5 days of black tarry stools. Two years prior, she was diagnosed with pancreatic head adenocarcinoma and underwent a pancreaticoduodenectomy with portal vein reconstruction. Subsequent CT scans demonstrated post surgical portal vein stenosis. On admission, she denied fevers, abdominal pain, or hematemesis. Labs were notable for a hemoglobin of 5.7 g/dl, INR of 1.6, and bilirubin of 1.0 mg/dl. Physical exam demonstrated an abdominal fluid wave and melena on digital rectal exam. CT abdomen showed post Whipple anatomy, severe portal vein stenosis, large volume ascites, and extensive upper abdominal collaterals including peri-portal and peri-biliary varices. Upper endoscopy revealed blood in the afferent jejunal limb. Bleeding was found to be originating from the choledochojejunostomy. Multiple large visible vessels with stigmata of recent bleeding were visualized within the common bile duct. A single hemostatic clip was placed on one of the vessels, resulting in increased bleeding. Hemostasis was achieved with cyanoacrylate injection. The patient was transferred to the interventional radiology suite, where she underwent portal venography confirming severe stenosis of the porto-mesenteric confluence. Interventional radiology performed portal vein balloon dilation and stent placement. The patient had no further bleeding following the procedure.
Discussion: Bleeding from peri-biliary varices is a rare cause of upper GI bleeding. In this case, non cirrhotic portal hypertension from acquired portal vein stenosis after pancreaticoduodenectomy led to clinically significant gastrointestinal bleeding. Portal biliopathy is an uncommon and late presentation in patients with extrahepatic portal vein obstruction. In many cases, patients present with signs and symptoms of biliary obstruction. Treatment of PB should involve a multidisciplinary discussion among various subspecialties including gastroenterology, interventional radiology, and hepatobiliary surgery.
Disclosures:
Zuhair Sadiq, BA1, Khalifa Bshesh, BA1, Michael J. Mintz, MD2, Malorie Simons, MD2, Allison Yang, MD3. E0057 - Portal Biliopathy in a Patient Who Underwent a Whipple Procedure With Portal Vein Reconstruction, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Weill Cornell Medical College, New York, NY; 2New York-Presbyterian Hospital/Weill Cornell Medicine, New York, NY; 3New York Presbyterian Hospital/ Weill Cornell Medicine, New York, NY
Introduction: Portal biliopathy is a condition that is defined as abnormalities in the biliary tract due to portal hypertension. Some patients may present with abdominal pain, fever, jaundice, or pruritis. Rarely, portal hypertension secondary to portal vein abnormalities cause peri-biliary varices. We report a case of a patient with a peri-biliary variceal bleed due to portal hypertension from acquired portal vein stenosis.
Case Description/Methods: A 59-year-old female with a past medical history of pancreatic ductal adenocarcinoma presented to the hospital with 5 days of black tarry stools. Two years prior, she was diagnosed with pancreatic head adenocarcinoma and underwent a pancreaticoduodenectomy with portal vein reconstruction. Subsequent CT scans demonstrated post surgical portal vein stenosis. On admission, she denied fevers, abdominal pain, or hematemesis. Labs were notable for a hemoglobin of 5.7 g/dl, INR of 1.6, and bilirubin of 1.0 mg/dl. Physical exam demonstrated an abdominal fluid wave and melena on digital rectal exam. CT abdomen showed post Whipple anatomy, severe portal vein stenosis, large volume ascites, and extensive upper abdominal collaterals including peri-portal and peri-biliary varices. Upper endoscopy revealed blood in the afferent jejunal limb. Bleeding was found to be originating from the choledochojejunostomy. Multiple large visible vessels with stigmata of recent bleeding were visualized within the common bile duct. A single hemostatic clip was placed on one of the vessels, resulting in increased bleeding. Hemostasis was achieved with cyanoacrylate injection. The patient was transferred to the interventional radiology suite, where she underwent portal venography confirming severe stenosis of the porto-mesenteric confluence. Interventional radiology performed portal vein balloon dilation and stent placement. The patient had no further bleeding following the procedure.
Discussion: Bleeding from peri-biliary varices is a rare cause of upper GI bleeding. In this case, non cirrhotic portal hypertension from acquired portal vein stenosis after pancreaticoduodenectomy led to clinically significant gastrointestinal bleeding. Portal biliopathy is an uncommon and late presentation in patients with extrahepatic portal vein obstruction. In many cases, patients present with signs and symptoms of biliary obstruction. Treatment of PB should involve a multidisciplinary discussion among various subspecialties including gastroenterology, interventional radiology, and hepatobiliary surgery.
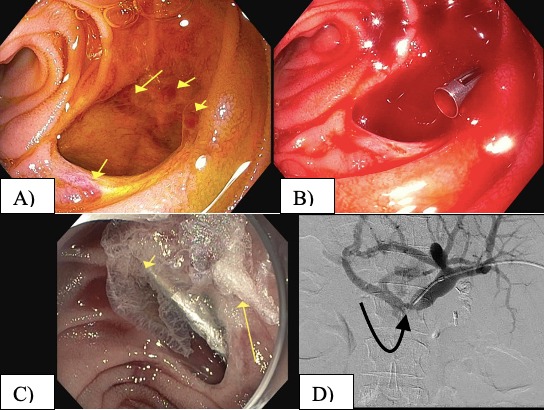
Figure: Figure 1: A. Choledochojejunostomy with visible varices. B. Hemostatic clip placement with subsequent bleeding. C. Injection of cyanoacrylate glue with hemostasis. D. Portal venography demonstrating portal vein stenosis at the porto-mesenteric confluence
Disclosures:
Zuhair Sadiq indicated no relevant financial relationships.
Khalifa Bshesh indicated no relevant financial relationships.
Michael Mintz indicated no relevant financial relationships.
Malorie Simons indicated no relevant financial relationships.
Allison Yang indicated no relevant financial relationships.
Zuhair Sadiq, BA1, Khalifa Bshesh, BA1, Michael J. Mintz, MD2, Malorie Simons, MD2, Allison Yang, MD3. E0057 - Portal Biliopathy in a Patient Who Underwent a Whipple Procedure With Portal Vein Reconstruction, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
