Back

Poster Session E - Tuesday Afternoon
Category: Biliary/Pancreas
E0058 - Delayed Gastrointestinal Hemorrhage From Visceral Artery Pseudoaneurysm in Necrotizing Pancreatitis After LAMS Removal
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Fatima Khan, MD
Yale University School of Medicine
New Haven, CT
Presenting Author(s)
Fatima Khan, MD, Thiruvengadam Muniraj, MD, PhD, Darrick K. Li, MD, PhD
Yale University School of Medicine, New Haven, CT
Introduction: Delayed bleeding from visceral artery pseudoaneurysm (PA) formation is an uncommon complication of lumen-apposing metal stent (LAMS) placement. Risk factors for gastrointestinal bleeding (GIB) in patients with LAMS remain largely undefined. We report a case of delayed GIB due to rupture of a splenic artery PA 16 months after LAMS removal.
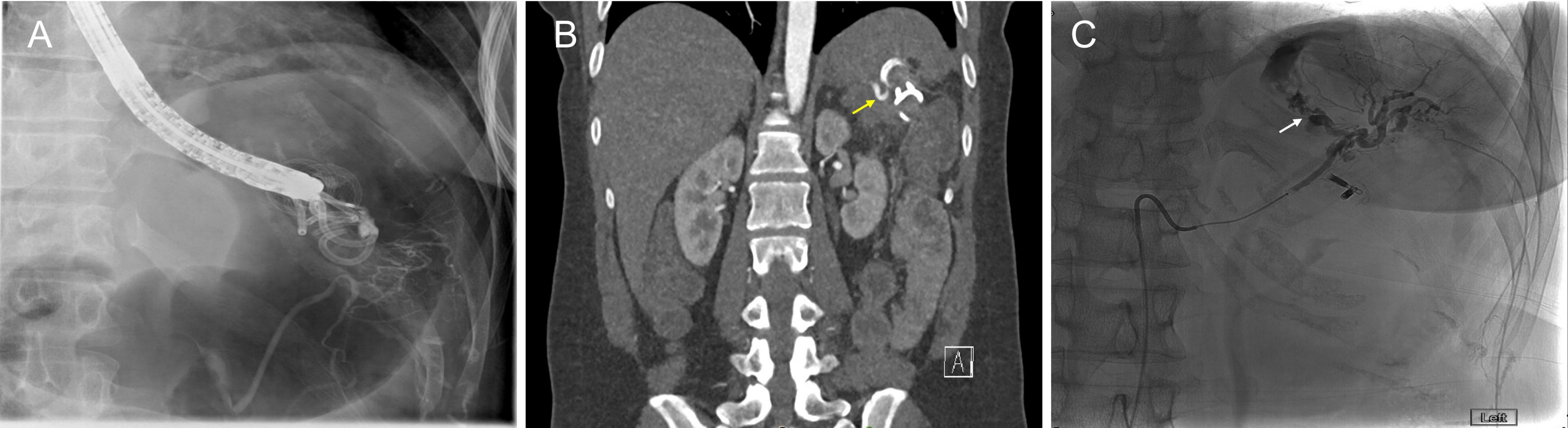
Case Description/Methods: A 34-year-old female with a history of severe necrotizing pancreatitis presented to our hospital with massive hematemesis. 23 months prior to presentation, she underwent uncomplicated placement of a 15x10 mm LAMS and two 7 Fr x 4 cm double pigtail plastic stents for drainage of walled-off pancreatic necrosis. She was briefly lost to follow-up and returned for LAMS removal 5 months later. Contrast was injected into the residual cyst cavity and contrast filling was noted of what appeared to be a splenic vessel without active bleeding (Panel A). CT angiogram showed no PA but proximity of the splenic hilar vasculature to the LAMS (Panel B). The LAMS was successfully removed 2 months later without complication.
On presentation, she was tachycardic but normotensive. Laboratory studies were notable for hemoglobin 8.8 g/dL (baseline 14 g/dL). Upper endoscopy showed brisk bleeding in the proximal gastric body near the area of prior LAMS. Her bleeding was refractory to endoscopic hemostatic maneuvers, and she underwent emergent mesenteric angiography. Angiography revealed active arterial extravasation arising from the inferior segmental branch of the splenic artery (Panel C) which was successfully embolized with no further bleeding.
Discussion: Visceral artery PA development after LAMS placement is thought to occur due to friction of the inner flange against regional vasculature surrounding the necrotic cavity as it collapses. Close anatomical proximity of LAMS to regional vasculature increases the risk of PA development. In our case, the LAMS was placed near the rich vascular supply of the splenic hilum. Most reported bleeding events related to LAMS have occurred within eight weeks of placement. Our case is notable for the prolonged delay between LAMS removal and bleeding presentation. Adherent scar tissue between the gastric wall and vasculature could potentially cause delayed PA development after LAMS removal. This case reinforces that high clinical suspicion for PA bleeding is necessary for patients who have previously undergone distant LAMS removal who present with massive GIB.
Disclosures:
Fatima Khan, MD, Thiruvengadam Muniraj, MD, PhD, Darrick K. Li, MD, PhD. E0058 - Delayed Gastrointestinal Hemorrhage From Visceral Artery Pseudoaneurysm in Necrotizing Pancreatitis After LAMS Removal, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Yale University School of Medicine, New Haven, CT
Introduction: Delayed bleeding from visceral artery pseudoaneurysm (PA) formation is an uncommon complication of lumen-apposing metal stent (LAMS) placement. Risk factors for gastrointestinal bleeding (GIB) in patients with LAMS remain largely undefined. We report a case of delayed GIB due to rupture of a splenic artery PA 16 months after LAMS removal.
Case Description/Methods: A 34-year-old female with a history of severe necrotizing pancreatitis presented to our hospital with massive hematemesis. 23 months prior to presentation, she underwent uncomplicated placement of a 15x10 mm LAMS and two 7 Fr x 4 cm double pigtail plastic stents for drainage of walled-off pancreatic necrosis. She was briefly lost to follow-up and returned for LAMS removal 5 months later. Contrast was injected into the residual cyst cavity and contrast filling was noted of what appeared to be a splenic vessel without active bleeding (Panel A). CT angiogram showed no PA but proximity of the splenic hilar vasculature to the LAMS (Panel B). The LAMS was successfully removed 2 months later without complication.
On presentation, she was tachycardic but normotensive. Laboratory studies were notable for hemoglobin 8.8 g/dL (baseline 14 g/dL). Upper endoscopy showed brisk bleeding in the proximal gastric body near the area of prior LAMS. Her bleeding was refractory to endoscopic hemostatic maneuvers, and she underwent emergent mesenteric angiography. Angiography revealed active arterial extravasation arising from the inferior segmental branch of the splenic artery (Panel C) which was successfully embolized with no further bleeding.
Discussion: Visceral artery PA development after LAMS placement is thought to occur due to friction of the inner flange against regional vasculature surrounding the necrotic cavity as it collapses. Close anatomical proximity of LAMS to regional vasculature increases the risk of PA development. In our case, the LAMS was placed near the rich vascular supply of the splenic hilum. Most reported bleeding events related to LAMS have occurred within eight weeks of placement. Our case is notable for the prolonged delay between LAMS removal and bleeding presentation. Adherent scar tissue between the gastric wall and vasculature could potentially cause delayed PA development after LAMS removal. This case reinforces that high clinical suspicion for PA bleeding is necessary for patients who have previously undergone distant LAMS removal who present with massive GIB.
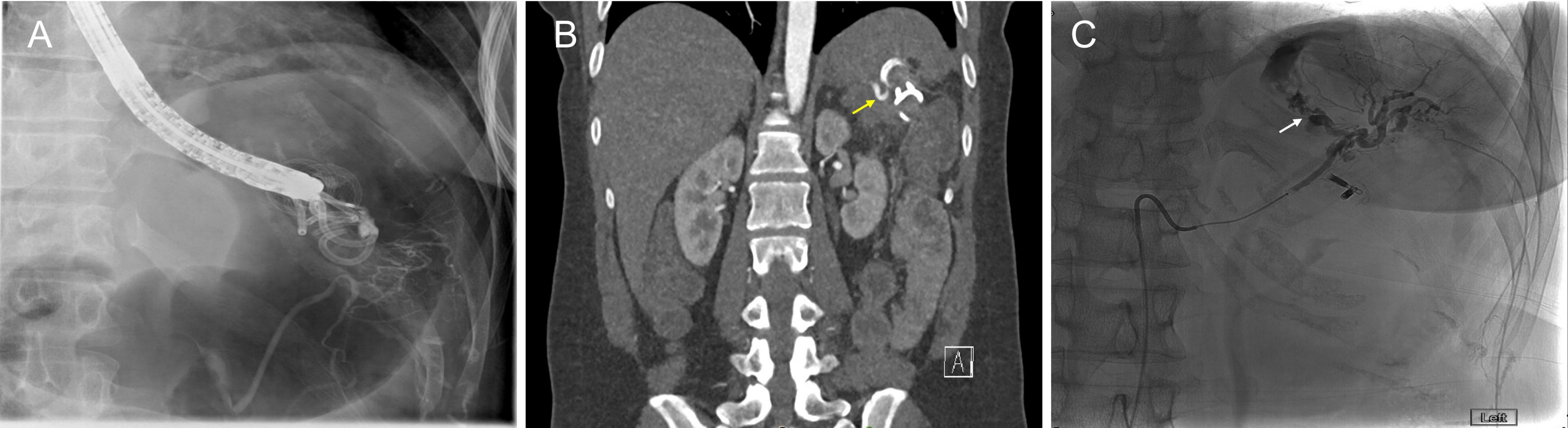
Figure: (A) Fluoroscopic image of contrast injection into residual cyst cavity demonstrating opacification of likely splenic vasculature; (B) Coronal images demonstrating the proximity of the LAMS to the vasculature of the splenic hilum (yellow arrow); (C) Super-selective angiography demonstrating active extravasation into the lateral aspect of the stomach from a pseudoaneurysm (white arrow) involving an inferior segmental branch of the splenic artery.
Disclosures:
Fatima Khan indicated no relevant financial relationships.
Thiruvengadam Muniraj indicated no relevant financial relationships.
Darrick Li indicated no relevant financial relationships.
Fatima Khan, MD, Thiruvengadam Muniraj, MD, PhD, Darrick K. Li, MD, PhD. E0058 - Delayed Gastrointestinal Hemorrhage From Visceral Artery Pseudoaneurysm in Necrotizing Pancreatitis After LAMS Removal, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
