Back

Poster Session A - Sunday Afternoon
Category: Biliary/Pancreas
A0043 - IgG4-Seronegative Autoimmune Cholangiopathy With Pancreatic and Hepatic Involvement Mimicking as Primary Sclerosing Cholangitis
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio
- SA
Sudharshan Achalu, BA
Stanford University
Redwood City, CA
Presenting Author(s)
Sudharshan Achalu, BA1, Mike Wei, MD2, Rani Berry, MD3, Subhas Banerjee, MD3, Pejman Ghanouni, MD3, Paul Kwo, MD4
1Stanford University, Redwood City, CA; 2Stanford University School of Medicine, Palo Alto, CA; 3Stanford, Palo Alto, CA; 4Stanford University University School of Medicine, Redwood City, CA
Introduction: IgG4-seronegative autoimmune cholangiopathy is a rare cause of biliary strictures.
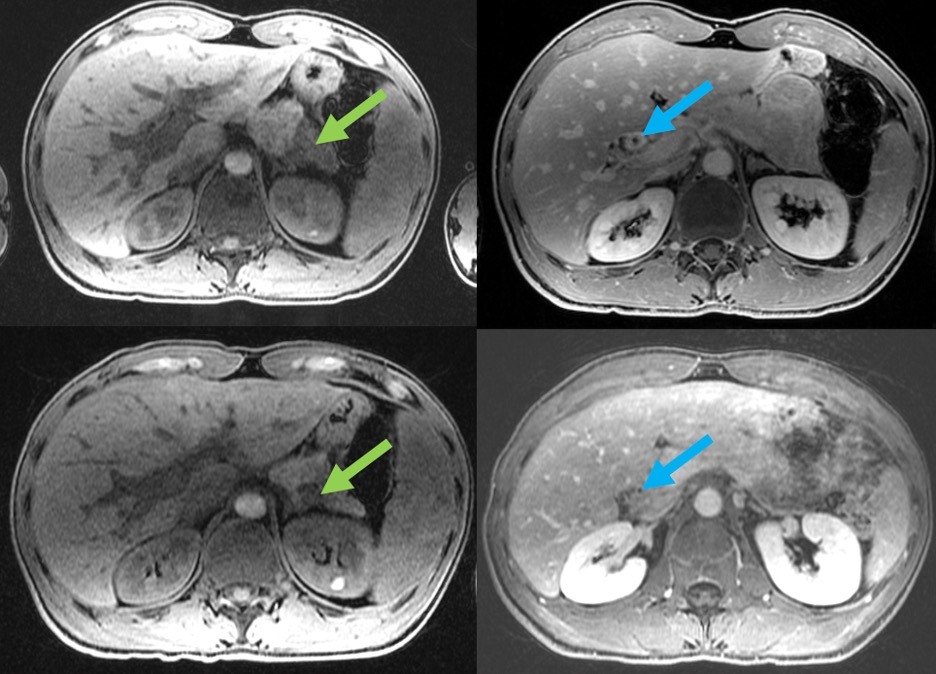
Case Description/Methods: 27-year-old male presented in 2011 with 4 months of abdominal bloating and cholestatic elevation of liver enzymes. MRI showed attenuated intra/extrahepatic ducts with beading, consistent with PSC. He was lost to follow up until 2017, when he presented with fever concerning for cholangitis. All autoimmune serologies were negative (ANA, SMA, AMA, pANCA, ASLA, LKM), and Total IgG and IgG4 were normal. ERCP showed a diffusely diseased biliary system characterized by thin, irregular, beaded ducts without dominant stricture, consistent with PSC. A liver biopsy was negative for features of autoimmune hepatitis and IgG4-related disease with negative IgG4 staining. He subsequently had multiple hospitalizations for cholangitis with bacteremia. MRCP at that time showed new focal stricture/intrahepatic biliary dilatation, and ERCP showed a common hepatic duct stricture extending into the left main hepatic duct that required stenting with multiple exchanges. Due to recurrent bouts of cholangitis with bacteremia, he was listed for liver transplantation for PSC in 2020 with intent to undergo live donor transplant. In 2021, MRCP showed a new T2 moderately hyperintense, T1 hypointense appearance of the distal 4 cm of the pancreatic tail with early hypoenhancement and delayed hyperenhancement suggestive of inflammation and fibrosis with marked periductal enhancement of the common hepatic duct with stenosis definitive for sclerosing cholangitis. Endoscopic ultrasound with fine needle biopsy failed to obtain sufficient tissue sample. These diagnostic studies suggested IgG4-seronegative autoimmune cholangiopathy with pancreatic involvement rather than PSC. Three weeks after initiation of prednisone, his liver tests showed substantial improvement in alkaline phosphatase and ALT, MRI showed improvement of biliary wall thickening, and follow-up ERCP showed improvement in biliary strictures (Figure 1); all stents were removed. He is no longer pursing live donor transplantation and he remains stable on azathioprine and low dose prednisone.
Discussion: IgG4-seronegative autoimmune cholangiopathy is a treatable though rare cause of biliary strictures that should be considered in those who present with morphologic changes of PSC. The diagnosis was considered when MRI revealed pancreatic inflammatory changes in addition to the biliary strictures.
Disclosures:
Sudharshan Achalu, BA1, Mike Wei, MD2, Rani Berry, MD3, Subhas Banerjee, MD3, Pejman Ghanouni, MD3, Paul Kwo, MD4. A0043 - IgG4-Seronegative Autoimmune Cholangiopathy With Pancreatic and Hepatic Involvement Mimicking as Primary Sclerosing Cholangitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Stanford University, Redwood City, CA; 2Stanford University School of Medicine, Palo Alto, CA; 3Stanford, Palo Alto, CA; 4Stanford University University School of Medicine, Redwood City, CA
Introduction: IgG4-seronegative autoimmune cholangiopathy is a rare cause of biliary strictures.
Case Description/Methods: 27-year-old male presented in 2011 with 4 months of abdominal bloating and cholestatic elevation of liver enzymes. MRI showed attenuated intra/extrahepatic ducts with beading, consistent with PSC. He was lost to follow up until 2017, when he presented with fever concerning for cholangitis. All autoimmune serologies were negative (ANA, SMA, AMA, pANCA, ASLA, LKM), and Total IgG and IgG4 were normal. ERCP showed a diffusely diseased biliary system characterized by thin, irregular, beaded ducts without dominant stricture, consistent with PSC. A liver biopsy was negative for features of autoimmune hepatitis and IgG4-related disease with negative IgG4 staining. He subsequently had multiple hospitalizations for cholangitis with bacteremia. MRCP at that time showed new focal stricture/intrahepatic biliary dilatation, and ERCP showed a common hepatic duct stricture extending into the left main hepatic duct that required stenting with multiple exchanges. Due to recurrent bouts of cholangitis with bacteremia, he was listed for liver transplantation for PSC in 2020 with intent to undergo live donor transplant. In 2021, MRCP showed a new T2 moderately hyperintense, T1 hypointense appearance of the distal 4 cm of the pancreatic tail with early hypoenhancement and delayed hyperenhancement suggestive of inflammation and fibrosis with marked periductal enhancement of the common hepatic duct with stenosis definitive for sclerosing cholangitis. Endoscopic ultrasound with fine needle biopsy failed to obtain sufficient tissue sample. These diagnostic studies suggested IgG4-seronegative autoimmune cholangiopathy with pancreatic involvement rather than PSC. Three weeks after initiation of prednisone, his liver tests showed substantial improvement in alkaline phosphatase and ALT, MRI showed improvement of biliary wall thickening, and follow-up ERCP showed improvement in biliary strictures (Figure 1); all stents were removed. He is no longer pursing live donor transplantation and he remains stable on azathioprine and low dose prednisone.
Discussion: IgG4-seronegative autoimmune cholangiopathy is a treatable though rare cause of biliary strictures that should be considered in those who present with morphologic changes of PSC. The diagnosis was considered when MRI revealed pancreatic inflammatory changes in addition to the biliary strictures.
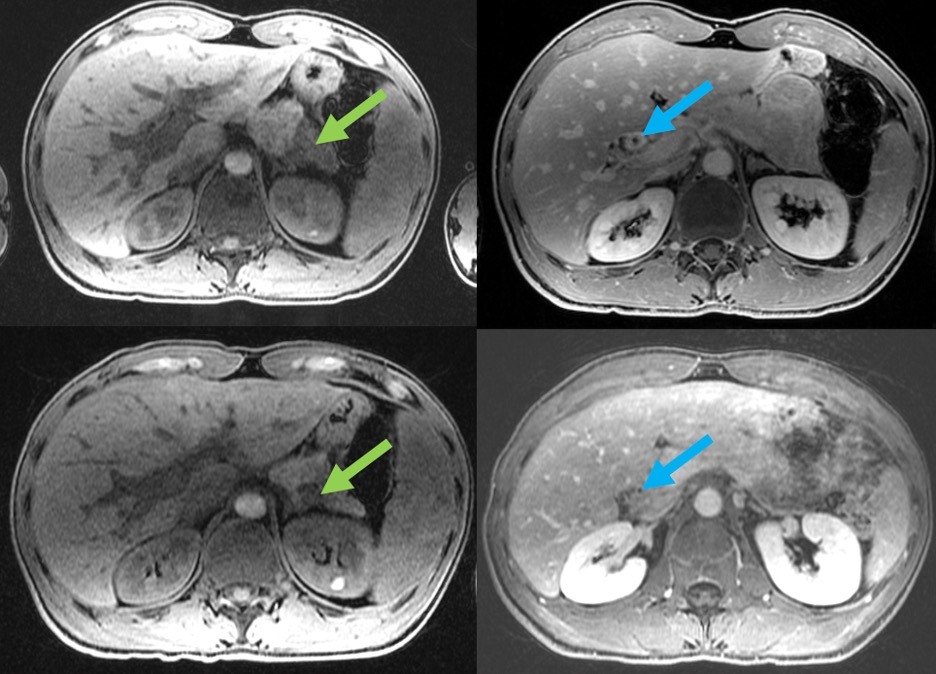
Figure: Left, top: Axial T1 weighted pre-contrast fat-suppressed image reveals sharply demarcated abnormal hypointense T1 signal in the pancreatic tail (green arrow). Right, top: Delayed post-contrast T1 weighted fat-suppressed image demonstrates marked peribiliary thickening and enhancement around the common hepatic duct (blue arrow). Left, bottom: Axial T1 weighted pre-contrast fat-suppressed image obtained 6 months after initiation of steroids shows normalization of T1 signal in the pancreatic tail (green arrow). Right, bottom: Delayed post-contrast T1 weighted fat-suppressed image obtained 6 months after initiation of steroids demonstrates resolution of peribiliary thickening and enhancement around the common hepatic duct (blue arrow)
Disclosures:
Sudharshan Achalu indicated no relevant financial relationships.
Mike Wei: AgilTx – Consultant. Neptune Medical, Inc – Consultant.
Rani Berry: metaMe – Advisor or Review Panel Member.
Subhas Banerjee: Boston Scientific – Consultant.
Pejman Ghanouni: HistoSonics – Consultant. INSIGHTEC – Advisory Committee/Board Member, Grant/Research Support. SonALAsense – Advisory Committee/Board Member, Stock-privately held company.
Paul Kwo: 89 Bio – Advisor or Review Panel Member. Abbvie – Advisory Committee/Board Member. Aligos – Advisor or Review Panel Member. Altimmune – Grant/Research Support. Ambyss – Advisor or Review Panel Member. Antios – Advisory Committee/Board Member. Arrowhead – Grant/Research Support. BMS – Grant/Research Support. Direct – Stock Options. Drug Farm – Advisor or Review Panel Member. Eiger – Grant/Research Support. Eisai – Advisor or Review Panel Member. Enact – Advisor or Review Panel Member. Gilead – Advisor or Review Panel Member, Grant/Research Support. Hepquant – Advisor or Review Panel Member. Inventiva – Advisor or Review Panel Member, Grant/Research Support. Janssen – Grant/Research Support. Lygenesis – Advisor or Review Panel Member. Mallinckrodt – Advisory Committee/Board Member. Novonordisk – Grant/Research Support. Surrozen – Advisor or Review Panel Member. Target registries – Grant/Research Support.
Sudharshan Achalu, BA1, Mike Wei, MD2, Rani Berry, MD3, Subhas Banerjee, MD3, Pejman Ghanouni, MD3, Paul Kwo, MD4. A0043 - IgG4-Seronegative Autoimmune Cholangiopathy With Pancreatic and Hepatic Involvement Mimicking as Primary Sclerosing Cholangitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
