Back

Poster Session C - Monday Afternoon
Category: Biliary/Pancreas
C0051 - A Young Immunocompetent Patient Presenting With Extrapulmonary Tuberculosis Complicated by Pancreatic Involvement Mimicking a Malignant Tumor
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Roshan Panchanathan, MD
University of Washington
Seattle, WA
Presenting Author(s)
Roshan Panchanathan, MD, Yutaka Tomizawa, MD, MSc
University of Washington, Seattle, WA
Introduction: Tuberculosis commonly affects the lungs and is communicable through respiratory droplets. Extrapulmonary Tuberculosis can involve almost any organ system but is much less common and often difficult to diagnose in the gastrointestinal tract.
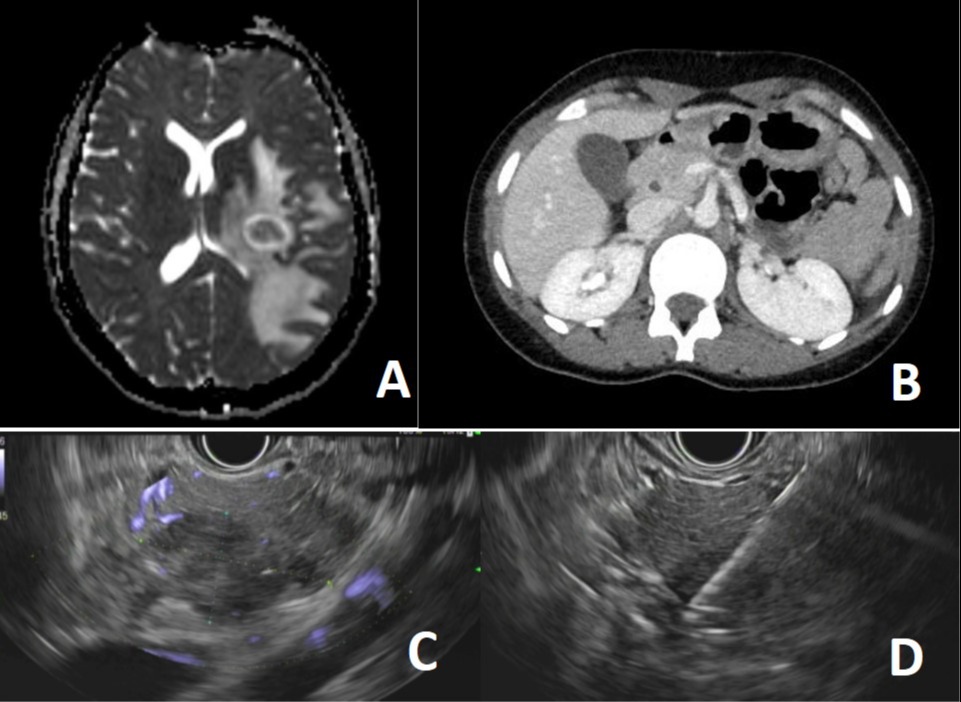
Case Description/Methods: A 24 year old Somali woman with no known past medical history experienced progressively worsening headaches associated with nausea and vomiting, as well as numerous small lesions on her left arm that eventually developed into large ulcerations. She subsequently had multiple falls associated with seizure-like movements and came to the United States to seek further care. MRI brain revealed rim-enhancing lesions with surrounding vasogenic edema (Figure A). CT abdomen and pelvis revealed an ill-defined 3.0 x 3.1 cm pancreatic head mass with mass effect on the portal vein and superior mesenteric vein, prominence of the common bile duct with abrupt cutoff (Figure B), and multiple enlarged thoracic lymph nodes. Endoscopic ultrasound (EUS) showed a poorly demarcated hypoechoic lesion with calcifications and focal necrosis in the pancreatic head (Figure C). Fine-needle biopsy was performed (Figure D). The remaining pancreatic parenchyma and duct appeared normal, and it was felt that the EUS findings were not typical malignant features. Cytopathology was negative for epithelial malignancy and revealed neutrophils with granulomatous inflammation. Further evaluation showed negative acid-fast bacilli (AFB) stains and Mycobacterium tuberculosis PCR, with an indeterminate non-TB Mycobacteria PCR. CA 19-9 and CEA were normal. Neuroradiology re-evaluated the MRI and felt atypical infection was a possible cause of the intracranial findings. Punch biopsy of her arm lesions revealed an ulcer with underlying necrotizing granulomatous inflammation. The multidisciplinary care team concluded her presentation was most consistent with extrapulmonary Tuberculosis given her necrotizing granulomas and prior residence in an endemic area. She was started on Rifampin, Isoniazid, Pyrazinamide, and Ethambutol.
Discussion: The diagnosis of extrapulmonary Tuberculosis can be challenging due to nonspecific symptoms and low sensitivity of the AFB stain. The most common sites include the bones, lymph nodes, and pleura, with the gastrointestinal organs much less frequently involved. Tissue biopsy of suspected lesions is helpful and can reveal granulomatous inflammation. Correlation with clinical, microbiological, laboratory, and radiologic findings is the key to diagnosis.
Disclosures:
Roshan Panchanathan, MD, Yutaka Tomizawa, MD, MSc. C0051 - A Young Immunocompetent Patient Presenting With Extrapulmonary Tuberculosis Complicated by Pancreatic Involvement Mimicking a Malignant Tumor, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
University of Washington, Seattle, WA
Introduction: Tuberculosis commonly affects the lungs and is communicable through respiratory droplets. Extrapulmonary Tuberculosis can involve almost any organ system but is much less common and often difficult to diagnose in the gastrointestinal tract.
Case Description/Methods: A 24 year old Somali woman with no known past medical history experienced progressively worsening headaches associated with nausea and vomiting, as well as numerous small lesions on her left arm that eventually developed into large ulcerations. She subsequently had multiple falls associated with seizure-like movements and came to the United States to seek further care. MRI brain revealed rim-enhancing lesions with surrounding vasogenic edema (Figure A). CT abdomen and pelvis revealed an ill-defined 3.0 x 3.1 cm pancreatic head mass with mass effect on the portal vein and superior mesenteric vein, prominence of the common bile duct with abrupt cutoff (Figure B), and multiple enlarged thoracic lymph nodes. Endoscopic ultrasound (EUS) showed a poorly demarcated hypoechoic lesion with calcifications and focal necrosis in the pancreatic head (Figure C). Fine-needle biopsy was performed (Figure D). The remaining pancreatic parenchyma and duct appeared normal, and it was felt that the EUS findings were not typical malignant features. Cytopathology was negative for epithelial malignancy and revealed neutrophils with granulomatous inflammation. Further evaluation showed negative acid-fast bacilli (AFB) stains and Mycobacterium tuberculosis PCR, with an indeterminate non-TB Mycobacteria PCR. CA 19-9 and CEA were normal. Neuroradiology re-evaluated the MRI and felt atypical infection was a possible cause of the intracranial findings. Punch biopsy of her arm lesions revealed an ulcer with underlying necrotizing granulomatous inflammation. The multidisciplinary care team concluded her presentation was most consistent with extrapulmonary Tuberculosis given her necrotizing granulomas and prior residence in an endemic area. She was started on Rifampin, Isoniazid, Pyrazinamide, and Ethambutol.
Discussion: The diagnosis of extrapulmonary Tuberculosis can be challenging due to nonspecific symptoms and low sensitivity of the AFB stain. The most common sites include the bones, lymph nodes, and pleura, with the gastrointestinal organs much less frequently involved. Tissue biopsy of suspected lesions is helpful and can reveal granulomatous inflammation. Correlation with clinical, microbiological, laboratory, and radiologic findings is the key to diagnosis.
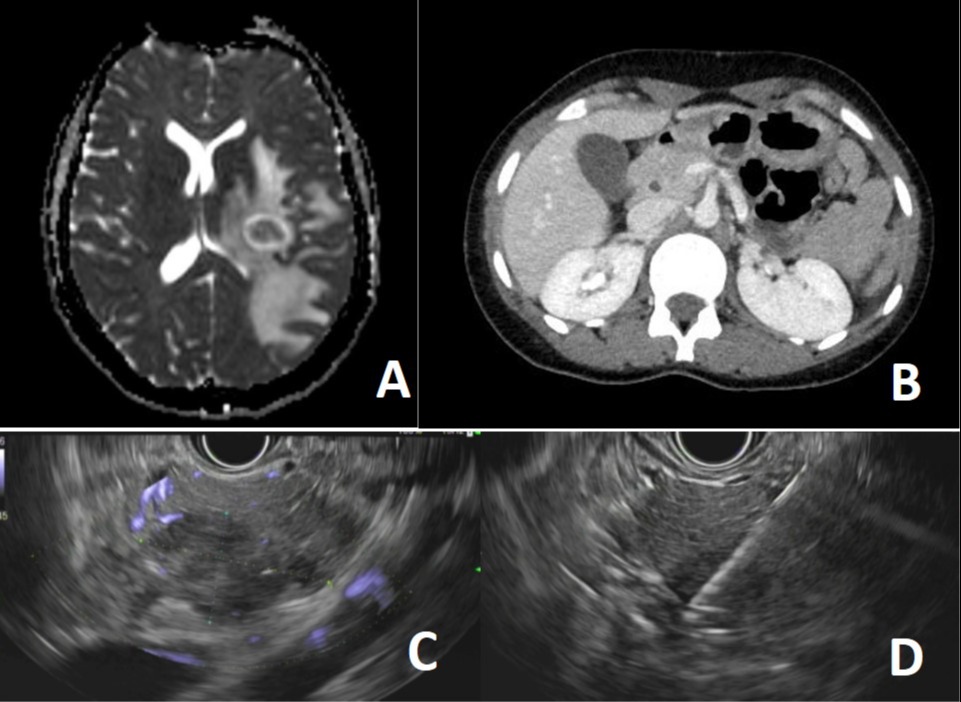
Figure: A) Rim-enhancing lesions with vasogenic edema B) Ill-defined pancreatic head mass with local mass effect C) Poorly demarcated hypoechoic pancreatic head lesion with calcifications and focal necrosis D) Fine-needle biopsy
Disclosures:
Roshan Panchanathan indicated no relevant financial relationships.
Yutaka Tomizawa indicated no relevant financial relationships.
Roshan Panchanathan, MD, Yutaka Tomizawa, MD, MSc. C0051 - A Young Immunocompetent Patient Presenting With Extrapulmonary Tuberculosis Complicated by Pancreatic Involvement Mimicking a Malignant Tumor, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

