Back

Poster Session E - Tuesday Afternoon
Category: Biliary/Pancreas
E0069 - Successful Treatment of a Complex Bile Leak With Endoclips During Percutaneously Necrosectomy
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Kelli C. Kosako Yost, MD
University of Arizona College of Medicine
Phoenix, AZ
Presenting Author(s)
Kelli C. Kosako Yost, MD1, Paul A. Muna Aguon, MD2, Sakolwan Suchartlikitwong, MD1, Nael Haddad, MD1, Nina Rawal, 3, Rawad Mounzer, MD4, Teodor C. Pitea, MD5, Qumber Ali, DO6
1University of Arizona College of Medicine, Phoenix, AZ; 2University of Arizona, Phoenix, AZ; 3Xavier College Preparatory School, Phoenix, AZ; 4Inverventional Endoscopy Associates, Phoenix, AZ; 5Interventional Endoscopy Associates, Scottsdale, AZ; 6University of Arizona College of Medicine - Phoenix Internal Medicine Residency, Phoenix, AZ
Introduction: Biliary injuries, such as bile leaks and fistulas, although rare, carry an increased risk of morbidity and mortality for patients. There are variable methods on how to proceed when one occurs, including stent placement and sphincterotomy via ERCP or percutaneous drainage. If these methods don’t succeed due to complexity or other factors, unconventional methods may be employed.
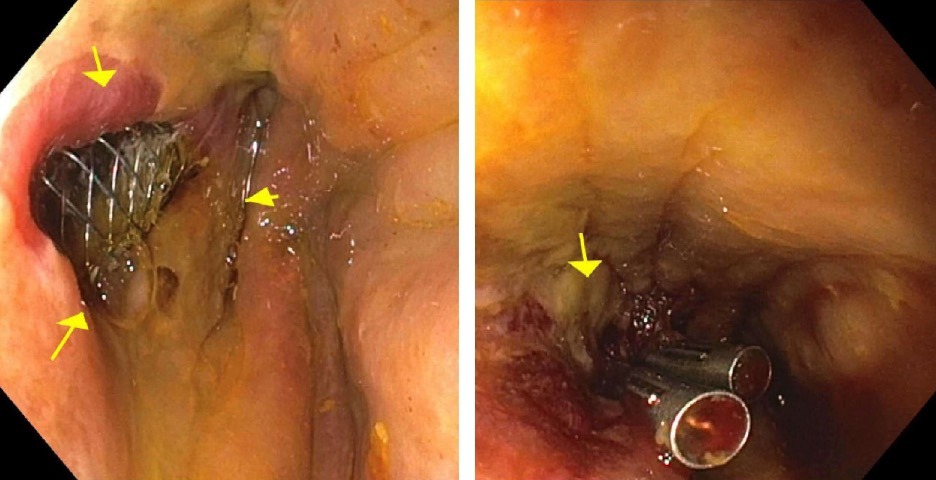
Case Description/Methods: A 36 y.o. male with a symptomatic cholelithiasis and choledocholithiasis underwent a laparoscopic cholecystectomy and ERCP with stone removal at an outside hospital. Patient continued to have smoldering abdominal pain after the procedure and EUS revealed a large peripancreatic necrotic collection with lipase >4000 and bilirubin of 14.5. ERCP showed a large caliber common hepatic duct leak and an 8mm x 8cm covered metal biliary stent was placed within the common bile duct, as well as an 18mm x 10cm covered esophageal stent was placed in the right lower quadrant, across the cystostomy, for percutaneous endoscopic necrosectomy. HIDA scan showed a persistent active bile leak near the location of the peripancreatic fluid collection. Necrosectomy was performed with successful clearance of the cavity. A concomitant 2cm bile duct wall defect was noted with exposure of the metal biliary stent. A dual approach with two endoclips were used to approximate the wall defect and a fully covered metal stent was left in the common bile duct to seal the defect from the inside and direct bile into the duodenum. The location of the defect on the common bile duct, not the cystic duct remnant, as well as the lack of visualization of leak on initial ERCP support that this was a fistula between the common bile duct and the peripancreatic fluid collection. Repeat ERCP at 3 and 5 months showed no further contrast extravasation and no bile duct stricture, and the metal stent was removed at 5 months.
Discussion: This case illustrates a novel approach that successfully treated a fistula between the bile duct and a pseudocyst with endoclips during a percutaneous necrosectomy. Although undocumented in the literature, complex, refractory biliary injuries require unconventional methods at times. This case proved successful in a young but very complicated patient and should be explored.
Disclosures:
Kelli C. Kosako Yost, MD1, Paul A. Muna Aguon, MD2, Sakolwan Suchartlikitwong, MD1, Nael Haddad, MD1, Nina Rawal, 3, Rawad Mounzer, MD4, Teodor C. Pitea, MD5, Qumber Ali, DO6. E0069 - Successful Treatment of a Complex Bile Leak With Endoclips During Percutaneously Necrosectomy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Arizona College of Medicine, Phoenix, AZ; 2University of Arizona, Phoenix, AZ; 3Xavier College Preparatory School, Phoenix, AZ; 4Inverventional Endoscopy Associates, Phoenix, AZ; 5Interventional Endoscopy Associates, Scottsdale, AZ; 6University of Arizona College of Medicine - Phoenix Internal Medicine Residency, Phoenix, AZ
Introduction: Biliary injuries, such as bile leaks and fistulas, although rare, carry an increased risk of morbidity and mortality for patients. There are variable methods on how to proceed when one occurs, including stent placement and sphincterotomy via ERCP or percutaneous drainage. If these methods don’t succeed due to complexity or other factors, unconventional methods may be employed.
Case Description/Methods: A 36 y.o. male with a symptomatic cholelithiasis and choledocholithiasis underwent a laparoscopic cholecystectomy and ERCP with stone removal at an outside hospital. Patient continued to have smoldering abdominal pain after the procedure and EUS revealed a large peripancreatic necrotic collection with lipase >4000 and bilirubin of 14.5. ERCP showed a large caliber common hepatic duct leak and an 8mm x 8cm covered metal biliary stent was placed within the common bile duct, as well as an 18mm x 10cm covered esophageal stent was placed in the right lower quadrant, across the cystostomy, for percutaneous endoscopic necrosectomy. HIDA scan showed a persistent active bile leak near the location of the peripancreatic fluid collection. Necrosectomy was performed with successful clearance of the cavity. A concomitant 2cm bile duct wall defect was noted with exposure of the metal biliary stent. A dual approach with two endoclips were used to approximate the wall defect and a fully covered metal stent was left in the common bile duct to seal the defect from the inside and direct bile into the duodenum. The location of the defect on the common bile duct, not the cystic duct remnant, as well as the lack of visualization of leak on initial ERCP support that this was a fistula between the common bile duct and the peripancreatic fluid collection. Repeat ERCP at 3 and 5 months showed no further contrast extravasation and no bile duct stricture, and the metal stent was removed at 5 months.
Discussion: This case illustrates a novel approach that successfully treated a fistula between the bile duct and a pseudocyst with endoclips during a percutaneous necrosectomy. Although undocumented in the literature, complex, refractory biliary injuries require unconventional methods at times. This case proved successful in a young but very complicated patient and should be explored.
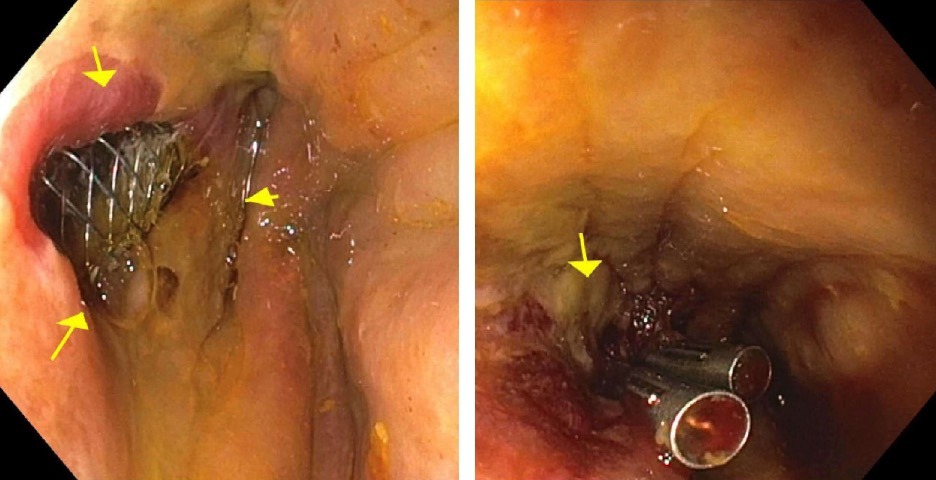
Figure: Endoscopic view of the 2cm bile duct wall defect via a percutaneous approach (Left) vs. the repaired defect with endoclips (Right)
Disclosures:
Kelli Kosako Yost indicated no relevant financial relationships.
Paul Muna Aguon indicated no relevant financial relationships.
Sakolwan Suchartlikitwong indicated no relevant financial relationships.
Nael Haddad indicated no relevant financial relationships.
Nina Rawal indicated no relevant financial relationships.
Rawad Mounzer indicated no relevant financial relationships.
Teodor Pitea indicated no relevant financial relationships.
Qumber Ali indicated no relevant financial relationships.
Kelli C. Kosako Yost, MD1, Paul A. Muna Aguon, MD2, Sakolwan Suchartlikitwong, MD1, Nael Haddad, MD1, Nina Rawal, 3, Rawad Mounzer, MD4, Teodor C. Pitea, MD5, Qumber Ali, DO6. E0069 - Successful Treatment of a Complex Bile Leak With Endoclips During Percutaneously Necrosectomy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
