Back

Poster Session E - Tuesday Afternoon
Category: Biliary/Pancreas
E0070 - Mesenteric Vasculitis Presenting as a Pancreatic Pseudoaneurysm Originating From the Superior Mesenteric Artery
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Kelli C. Kosako Yost, MD
University of Arizona College of Medicine
Phoenix, AZ
Presenting Author(s)
Kelli C. Kosako Yost, MD1, Wahid Wassef, MD, MPH, FACG1, Cole Mendenhall, MD1, Trent Smith, MD1, Qumber Ali, DO2
1University of Arizona College of Medicine, Phoenix, AZ; 2University of Arizona College of Medicine - Phoenix Internal Medicine Residency, Phoenix, AZ
Introduction: Pseudoaneurysms form at the site of an arterial injury due to blood extravasating into the surrounding tissues and have a propensity to rupture as they do not involve any layer of the vessel wall. In the pancreaticobiliary system, they almost always occur in conjunction with pancreatitis, surgery, or trauma. Other causes, like vasculitis, are extremely rare. Approximately 60-65% of cases of pancreatic pseudoaneurysms originate from the splenic artery, 20-25% from the gastroduodenal artery, 5-10% from the hepatic artery, and less than 5% from the left gastric arteries. After diagnosis on CT, pseudoaneurysms necessitate treatment, most typically with coil embolization or stenting by interventional radiology.
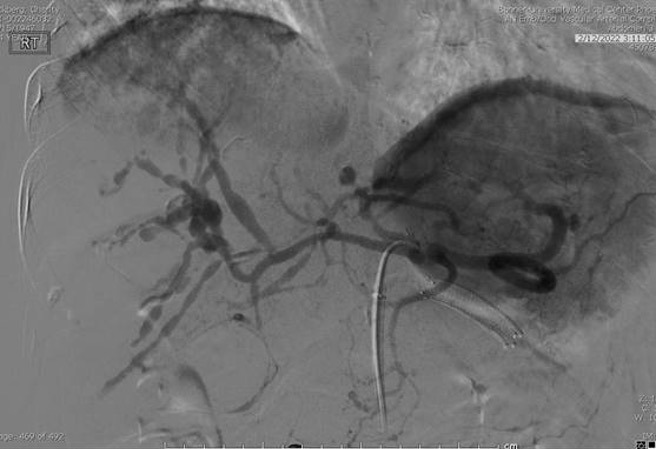
Case Description/Methods: A 74 y.o female with a past medical history of hypertension, Parkinson’s disease, and chronic pain presented with a 3-day history of jaundice, with subsequent lab workup revealing bilirubin 12.3 mg/dL, AST 238, ALT 18, alkaline phosphatase 760, and CA19-9 4087 u/mL. CT abdomen revealed a 9.5 x 5.5 x 6.5 cm mesenteric area pseudoaneurysm with 2.1 cm central arterial extravasation with a thick thrombus which surrounded the pancreatic head and neck and compressed the common bile duct, resulting in distal biliary obstruction. CT angiography was performed and showed innumerable mesenteric, intrahepatic, and intrasplenic pseudoaneurysms. Interventional radiology was consulted for fluoroscopic-guided embolization of the pseudoaneurysms and the six largest aneurysms involving the superior mesenteric artery were both stented and coil-embolized. The patient was treated with adjuvant prednisone and a repeat CT one month later showed resolution of the hematoma.
Discussion: This case illustrates a rare entity: a pancreatic pseudoaneurysm originating from the superior mesenteric artery that developed without typical predisposing factors, but due to an underlying systemic vasculitis. This case enforces that the gold standard for diagnosis of both visceral pseudoaneurysms and vasculitis is CT angiography, as the diffuse nature of the mesenteric pseudoaneurysms was not evident until angiography was utilized. This case challenges typical treatments for pseudoaneurysms, as an aggressive approach of both stenting and transcatheter coil embolization of large vascular territories was used and resulted in resolution of the pancreatic pseudocyst with no evidence of bowel infarction, despite the aggressive therapy.
Disclosures:
Kelli C. Kosako Yost, MD1, Wahid Wassef, MD, MPH, FACG1, Cole Mendenhall, MD1, Trent Smith, MD1, Qumber Ali, DO2. E0070 - Mesenteric Vasculitis Presenting as a Pancreatic Pseudoaneurysm Originating From the Superior Mesenteric Artery, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Arizona College of Medicine, Phoenix, AZ; 2University of Arizona College of Medicine - Phoenix Internal Medicine Residency, Phoenix, AZ
Introduction: Pseudoaneurysms form at the site of an arterial injury due to blood extravasating into the surrounding tissues and have a propensity to rupture as they do not involve any layer of the vessel wall. In the pancreaticobiliary system, they almost always occur in conjunction with pancreatitis, surgery, or trauma. Other causes, like vasculitis, are extremely rare. Approximately 60-65% of cases of pancreatic pseudoaneurysms originate from the splenic artery, 20-25% from the gastroduodenal artery, 5-10% from the hepatic artery, and less than 5% from the left gastric arteries. After diagnosis on CT, pseudoaneurysms necessitate treatment, most typically with coil embolization or stenting by interventional radiology.
Case Description/Methods: A 74 y.o female with a past medical history of hypertension, Parkinson’s disease, and chronic pain presented with a 3-day history of jaundice, with subsequent lab workup revealing bilirubin 12.3 mg/dL, AST 238, ALT 18, alkaline phosphatase 760, and CA19-9 4087 u/mL. CT abdomen revealed a 9.5 x 5.5 x 6.5 cm mesenteric area pseudoaneurysm with 2.1 cm central arterial extravasation with a thick thrombus which surrounded the pancreatic head and neck and compressed the common bile duct, resulting in distal biliary obstruction. CT angiography was performed and showed innumerable mesenteric, intrahepatic, and intrasplenic pseudoaneurysms. Interventional radiology was consulted for fluoroscopic-guided embolization of the pseudoaneurysms and the six largest aneurysms involving the superior mesenteric artery were both stented and coil-embolized. The patient was treated with adjuvant prednisone and a repeat CT one month later showed resolution of the hematoma.
Discussion: This case illustrates a rare entity: a pancreatic pseudoaneurysm originating from the superior mesenteric artery that developed without typical predisposing factors, but due to an underlying systemic vasculitis. This case enforces that the gold standard for diagnosis of both visceral pseudoaneurysms and vasculitis is CT angiography, as the diffuse nature of the mesenteric pseudoaneurysms was not evident until angiography was utilized. This case challenges typical treatments for pseudoaneurysms, as an aggressive approach of both stenting and transcatheter coil embolization of large vascular territories was used and resulted in resolution of the pancreatic pseudocyst with no evidence of bowel infarction, despite the aggressive therapy.
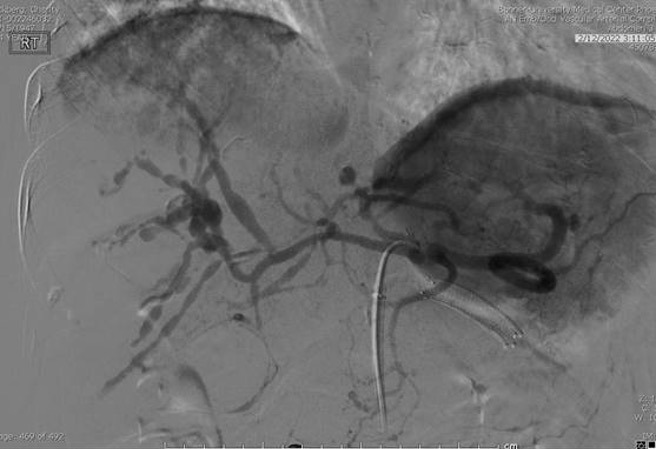
Figure: CT angiogram showing diffuse mesenteric pseudoaneurysms
Disclosures:
Kelli Kosako Yost indicated no relevant financial relationships.
Wahid Wassef indicated no relevant financial relationships.
Cole Mendenhall indicated no relevant financial relationships.
Trent Smith indicated no relevant financial relationships.
Qumber Ali indicated no relevant financial relationships.
Kelli C. Kosako Yost, MD1, Wahid Wassef, MD, MPH, FACG1, Cole Mendenhall, MD1, Trent Smith, MD1, Qumber Ali, DO2. E0070 - Mesenteric Vasculitis Presenting as a Pancreatic Pseudoaneurysm Originating From the Superior Mesenteric Artery, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
