Back

Poster Session A - Sunday Afternoon
Category: Biliary/Pancreas
A0061 - Purtscher Retinopathy: A Rare Clinical Manifestation of Acute Pancreatitis
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Nithya M. Yadlapalli, MD
UPMC
Cranberry Township, PA
Presenting Author(s)
Nithya M. Yadlapalli, MD1, Tiba Abdulwahid, MD2, Chris Musgrove, MD2, Rao Afzal, MD3, Fadi Francis, MD2, Evan Waxman, MD, PhD2
1UPMC, Cranberry Township, PA; 2UPMC, Pittsburgh, PA; 3UPMC, Cranberry township, PA
Introduction: Purtscher retinopathy was first described in patients with severe head trauma. Since its discovery it has since been associated with multiple clinical entities, including but not limited to acute pancreatitis and pancreatic adenocarcinoma. Purtscher and Purtscher- like retinopathy share similar pathophysiology and treatment and are collectively referred to as “Purtscher retinopathy”, the most commonly associated etiology includes trauma followed by acute pancreatitis. Purtscher retinopathy is extremely rare with a combined estimated incidence of 0.24 cases per million, thus lending to the utility of reporting such cases.
Case Description/Methods: A 64-year-old woman presents with mid-epigastric abdominal pain that alleviates with sitting forward, patient rates the pain 9/10 in severity with non-bilious emesis, diarrhea and poor oral intake. Initial lipase was 3230 U/L and CT of abdomen pelvis was remarkable for diffuse pancreatic edema with infiltration of peripancreatic fat. On Day 7 of hospitalization, she complained of decreased visual acuity with an inability to see color and count fingers. MRI revealed extensive white matter signal in bilateral occipital lobes suggestive of Posterior Reversible Encephalopathy Syndrome. Fundoscopic examination revealed cotton wool spots with intraretinal hemorrhages, suggestive of Purtscher-like retinopathy. Patient's vision improved throughout her hospital course with self-resolution of her acute pancreatitis.
Discussion:
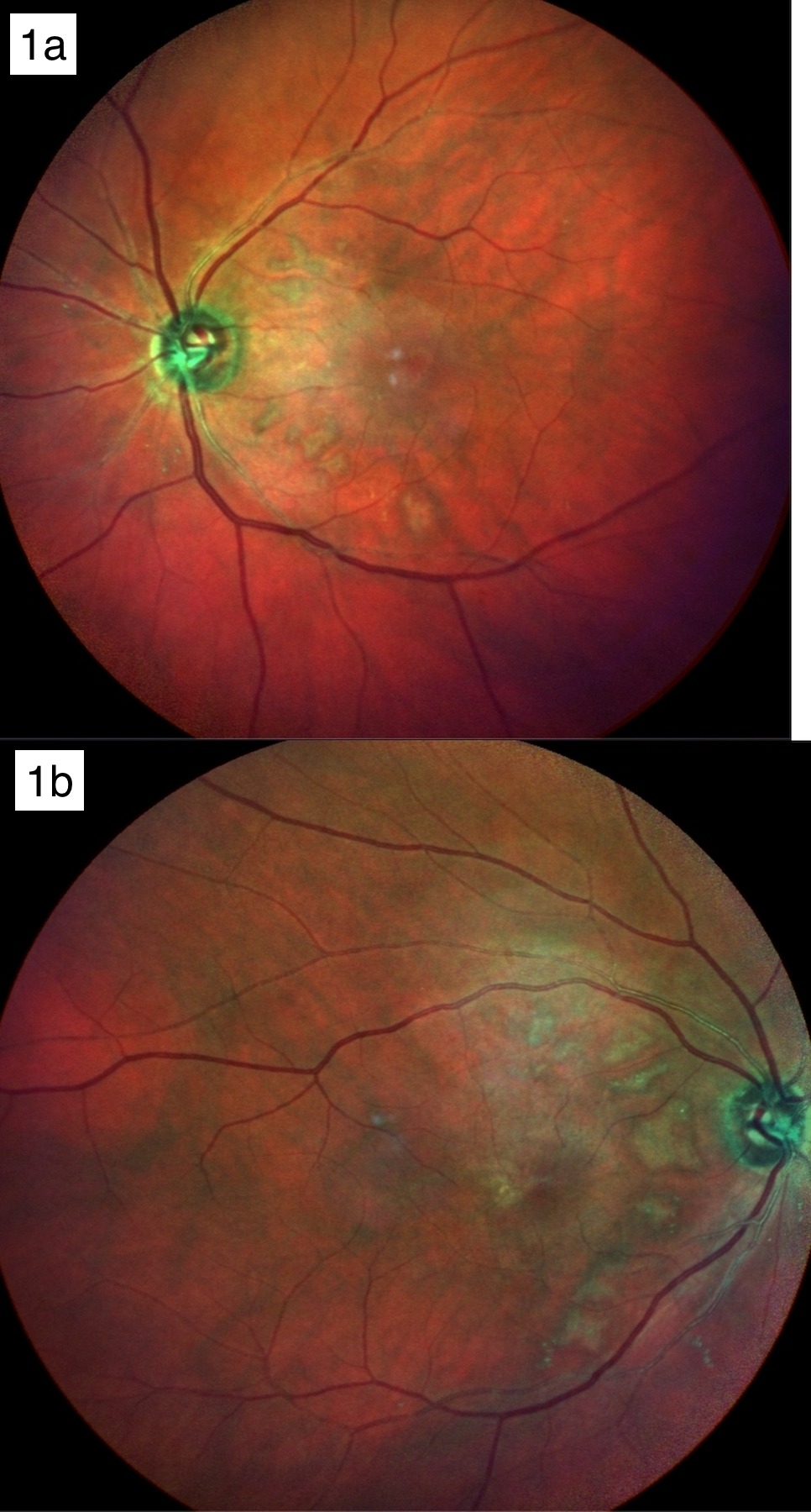
Pathogenesis of Purtscher retinopathy involves leucocyte aggregation induced by complement C5a activation with proteases in the setting of pancreatic injury. Leukoembolization results in arteriolar precapillary occlusion and ischemia of the microvascular bed in retinal vasculature. Fundoscopy is remarkable for cotton-wool spots with diffuse retinal whitening (Fig 1a, Fig 1b), hemorrhage and Purtscher flecken (capillary bed infarcts) which is pathognomonic. Systemic review identified 68 total cases of those 13 occurred secondary to acute pancreatitis. Prognosis for visual recovery is variable and currently there is no evidence-based guidelines regarding definitive treatment. Retinopathy associated with systemic vasculitis is controversially treated with high-dose corticosteroids, which failed to demonstrate statistically significant improvement in outcomes. Observation and treatment of underlying disease etiology demonstrates a judicious therapeutic option.
Disclosures:
Nithya M. Yadlapalli, MD1, Tiba Abdulwahid, MD2, Chris Musgrove, MD2, Rao Afzal, MD3, Fadi Francis, MD2, Evan Waxman, MD, PhD2. A0061 - Purtscher Retinopathy: A Rare Clinical Manifestation of Acute Pancreatitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1UPMC, Cranberry Township, PA; 2UPMC, Pittsburgh, PA; 3UPMC, Cranberry township, PA
Introduction: Purtscher retinopathy was first described in patients with severe head trauma. Since its discovery it has since been associated with multiple clinical entities, including but not limited to acute pancreatitis and pancreatic adenocarcinoma. Purtscher and Purtscher- like retinopathy share similar pathophysiology and treatment and are collectively referred to as “Purtscher retinopathy”, the most commonly associated etiology includes trauma followed by acute pancreatitis. Purtscher retinopathy is extremely rare with a combined estimated incidence of 0.24 cases per million, thus lending to the utility of reporting such cases.
Case Description/Methods: A 64-year-old woman presents with mid-epigastric abdominal pain that alleviates with sitting forward, patient rates the pain 9/10 in severity with non-bilious emesis, diarrhea and poor oral intake. Initial lipase was 3230 U/L and CT of abdomen pelvis was remarkable for diffuse pancreatic edema with infiltration of peripancreatic fat. On Day 7 of hospitalization, she complained of decreased visual acuity with an inability to see color and count fingers. MRI revealed extensive white matter signal in bilateral occipital lobes suggestive of Posterior Reversible Encephalopathy Syndrome. Fundoscopic examination revealed cotton wool spots with intraretinal hemorrhages, suggestive of Purtscher-like retinopathy. Patient's vision improved throughout her hospital course with self-resolution of her acute pancreatitis.
Discussion:
Pathogenesis of Purtscher retinopathy involves leucocyte aggregation induced by complement C5a activation with proteases in the setting of pancreatic injury. Leukoembolization results in arteriolar precapillary occlusion and ischemia of the microvascular bed in retinal vasculature. Fundoscopy is remarkable for cotton-wool spots with diffuse retinal whitening (Fig 1a, Fig 1b), hemorrhage and Purtscher flecken (capillary bed infarcts) which is pathognomonic. Systemic review identified 68 total cases of those 13 occurred secondary to acute pancreatitis. Prognosis for visual recovery is variable and currently there is no evidence-based guidelines regarding definitive treatment. Retinopathy associated with systemic vasculitis is controversially treated with high-dose corticosteroids, which failed to demonstrate statistically significant improvement in outcomes. Observation and treatment of underlying disease etiology demonstrates a judicious therapeutic option.
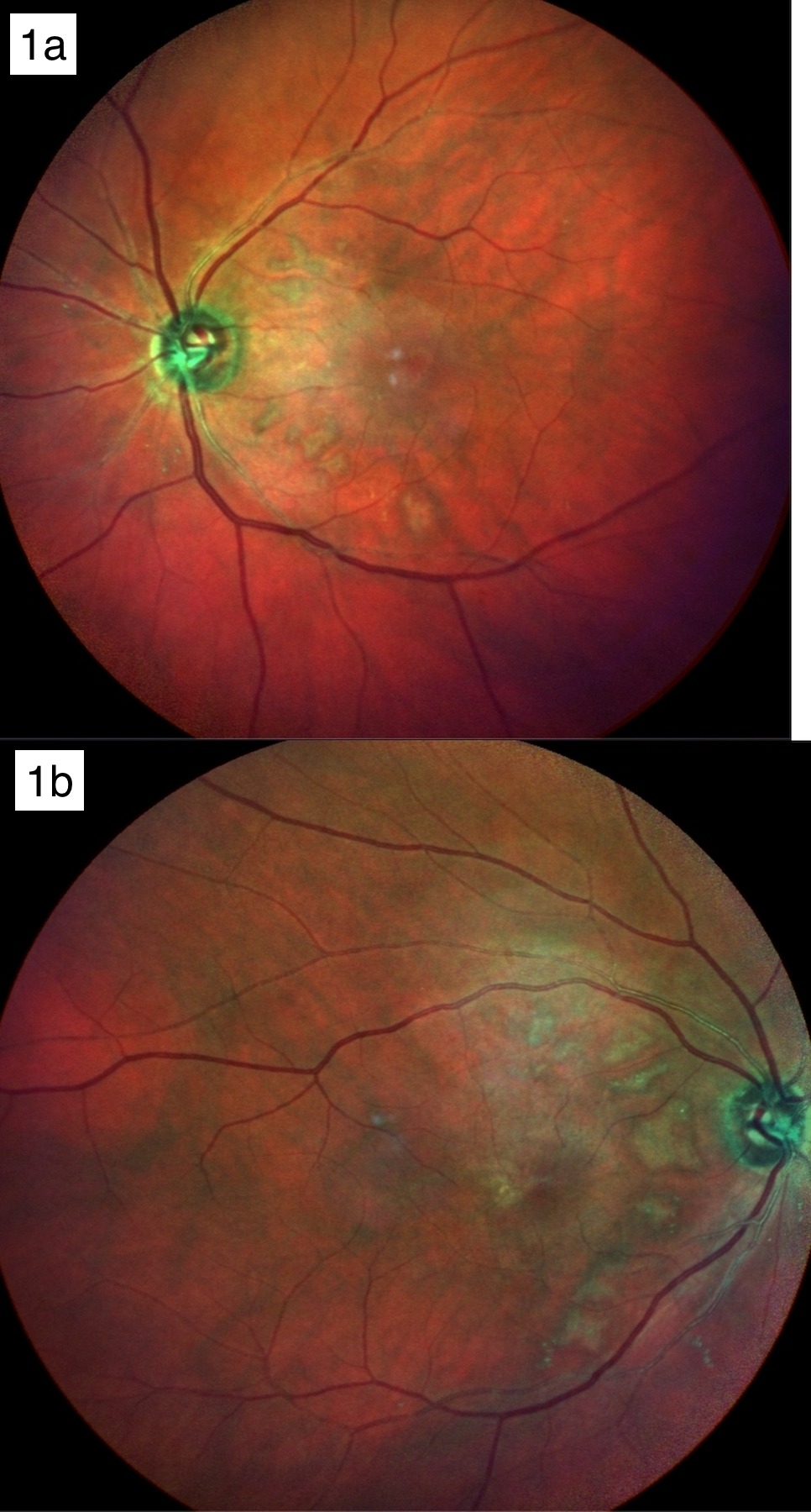
Figure: 1a. Residual patchy retinal whitening in nasal macula both eyes
1b. Residual patchy retinal whitening in nasal macula both eyes
1b. Residual patchy retinal whitening in nasal macula both eyes
Disclosures:
Nithya Yadlapalli indicated no relevant financial relationships.
Tiba Abdulwahid indicated no relevant financial relationships.
Chris Musgrove indicated no relevant financial relationships.
Rao Afzal indicated no relevant financial relationships.
Fadi Francis indicated no relevant financial relationships.
Evan Waxman indicated no relevant financial relationships.
Nithya M. Yadlapalli, MD1, Tiba Abdulwahid, MD2, Chris Musgrove, MD2, Rao Afzal, MD3, Fadi Francis, MD2, Evan Waxman, MD, PhD2. A0061 - Purtscher Retinopathy: A Rare Clinical Manifestation of Acute Pancreatitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
