Back

Poster Session B - Monday Morning
Category: Esophagus
B0222 - Acute Esophageal Necrosis: Low Flow Leading to Darkness
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Ayeetin Azah, MD, MBA
Walter Reed National Military Medical Center, MD
Presenting Author(s)
Ayeetin Azah, MD, MBA, Jared Magee, DO, MPH, Patrick Young, MD, FACG
Walter Reed National Military Medical Center, Bethesda, MD
Introduction: Acute esophageal necrosis (AEN), commonly referred to as black esophagus due to the striking circumferential blackening of the esophageal mucosa, is a rare clinical condition with a prevalence of up to 0.2%. The etiology of this condition is unclear but thought to involve the interplay of ischemia and gastric outlet obstruction with gastroesophageal reflux. As this condition carries with it a mortality rate of nearly 40%, prompt recognition and aggressive management is of the utmost importance to prevent perforation or stricture. Considering this, AEN should be recognized as a possible outcome of an ischemic event and considered a potential cause of spontaneous esophageal perforation.
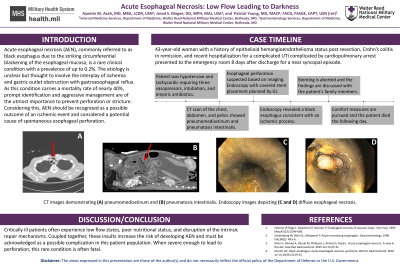
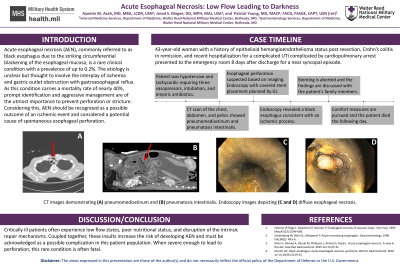
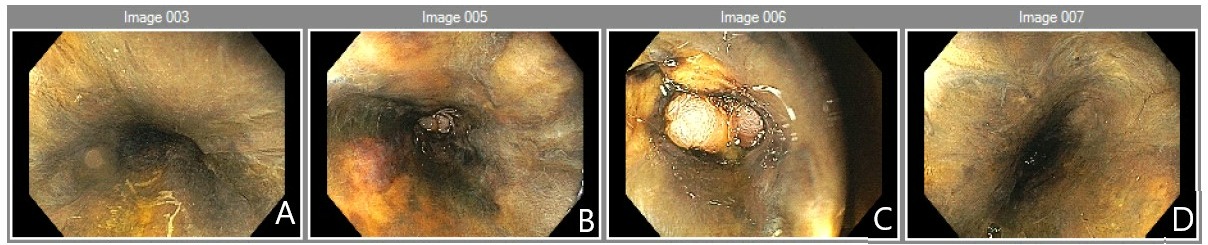
Case Description/Methods: A 43-year-old female with a history of epithelioid hemangioendothelioma status post resection, Crohn’s colitis in remission, and recent hospitalization for a complicated urinary tract infection and abdominopelvic ascites concerning for malignancy with hospitalization complicated by cardiopulmonary arrest presented to the emergency department 8 days after discharge following a near syncopal episode. She was found to be hypotensive with tachycardia concerning for shock. She was started on broad spectrum antibiotics, three vasopressors, intubated, and admitted to the ICU. A CT scan of her chest, abdomen, and pelvis showed extensive pneumomediastinum concerning for esophageal perforation and pneumatosis intestinalis. Perforation was confirmed utilizing serial chest x-rays with contrast demonstrating a right-sided esophageal leak at the gastroesophageal junction. Both cardiothoracic surgery and gastroenterology were consulted, she was not deemed a surgical candidate and endoscopy with covered stent placement was planned. Endoscopy revealed a black esophagus consistent with an ischemic process throughout the entire esophagus and pneumatosis intestinalis suggesting small bowel ischemia. Stenting was aborted and the findings were discussed with the patient’s family who decided to pursue comfort measures. The patient died the following day.
Discussion: It has been demonstrated that critically ill patients often experience low flow states, poor nutritional status, and disruption of intrinsic repair mechanisms. Coupled together, these insults increase the risk of developing AEN and must be acknowledged as a possible complication in this patient population. Although this is a rare condition, it should be recognized as a potential outcome of an ischemic event.
Disclosures:
Ayeetin Azah, MD, MBA, Jared Magee, DO, MPH, Patrick Young, MD, FACG. B0222 - Acute Esophageal Necrosis: Low Flow Leading to Darkness, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Walter Reed National Military Medical Center, Bethesda, MD
Introduction: Acute esophageal necrosis (AEN), commonly referred to as black esophagus due to the striking circumferential blackening of the esophageal mucosa, is a rare clinical condition with a prevalence of up to 0.2%. The etiology of this condition is unclear but thought to involve the interplay of ischemia and gastric outlet obstruction with gastroesophageal reflux. As this condition carries with it a mortality rate of nearly 40%, prompt recognition and aggressive management is of the utmost importance to prevent perforation or stricture. Considering this, AEN should be recognized as a possible outcome of an ischemic event and considered a potential cause of spontaneous esophageal perforation.
Case Description/Methods: A 43-year-old female with a history of epithelioid hemangioendothelioma status post resection, Crohn’s colitis in remission, and recent hospitalization for a complicated urinary tract infection and abdominopelvic ascites concerning for malignancy with hospitalization complicated by cardiopulmonary arrest presented to the emergency department 8 days after discharge following a near syncopal episode. She was found to be hypotensive with tachycardia concerning for shock. She was started on broad spectrum antibiotics, three vasopressors, intubated, and admitted to the ICU. A CT scan of her chest, abdomen, and pelvis showed extensive pneumomediastinum concerning for esophageal perforation and pneumatosis intestinalis. Perforation was confirmed utilizing serial chest x-rays with contrast demonstrating a right-sided esophageal leak at the gastroesophageal junction. Both cardiothoracic surgery and gastroenterology were consulted, she was not deemed a surgical candidate and endoscopy with covered stent placement was planned. Endoscopy revealed a black esophagus consistent with an ischemic process throughout the entire esophagus and pneumatosis intestinalis suggesting small bowel ischemia. Stenting was aborted and the findings were discussed with the patient’s family who decided to pursue comfort measures. The patient died the following day.
Discussion: It has been demonstrated that critically ill patients often experience low flow states, poor nutritional status, and disruption of intrinsic repair mechanisms. Coupled together, these insults increase the risk of developing AEN and must be acknowledged as a possible complication in this patient population. Although this is a rare condition, it should be recognized as a potential outcome of an ischemic event.
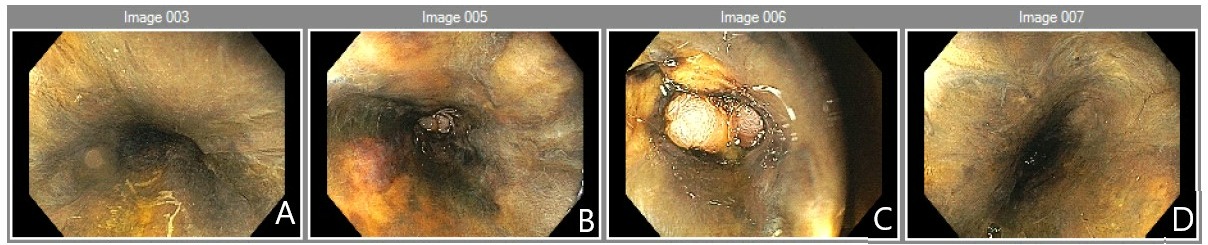
Figure: Images A-D depicts a diffusely abnormal mucosa throughout the esophagus, characterized by black/brown tissue consistent with ischemia.
Disclosures:
Ayeetin Azah indicated no relevant financial relationships.
Jared Magee indicated no relevant financial relationships.
Patrick Young indicated no relevant financial relationships.
Ayeetin Azah, MD, MBA, Jared Magee, DO, MPH, Patrick Young, MD, FACG. B0222 - Acute Esophageal Necrosis: Low Flow Leading to Darkness, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
