Back

Poster Session B - Monday Morning
Category: GI Bleeding
B0320 - Remnant Stomach Bleeding in Roux-en-Y Gastric Bypass Anatomy Managed by Transgastric Endoscopic Ultrasound-Guided Stenting and Hemostasis
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- MA
Mohammad Alqaisieh, MD
Mayo Clinic
Dalton, GA
Presenting Author(s)
Mohammad Alqaisieh, MD1, Karl Akiki, MD2, Tala Mahmoud, MD2, Andrew C. Storm, MD2
1Mayo Clinic, Dalton, GA; 2Mayo Clinic, Rochester, MN
Introduction: Upper GI bleeding identification and treatment is challenging in patients with Roux-en-Y gastric bypass (RYGB) due to their complex anatomy. Remnant stomach and duodenal bleeding in particular can be very challenging to reach and manage endoscopically due to the long length of the Roux and biliary limb.
Case Description/Methods: A 58-year-old female patient, who underwent gastric bypass in 2004, was diagnosed with fibular fracture and placed on NSAIDs 2 weeks before presenting to the hospital with melena and anemia. In addition to medical management of hypovolemic shock, the patient underwent upper endoscopy (EGD), colonoscopy, small bowel enteroscopy, and angiography followed by left gastric artery embolization all of which failed to localize or stop her bleeding.
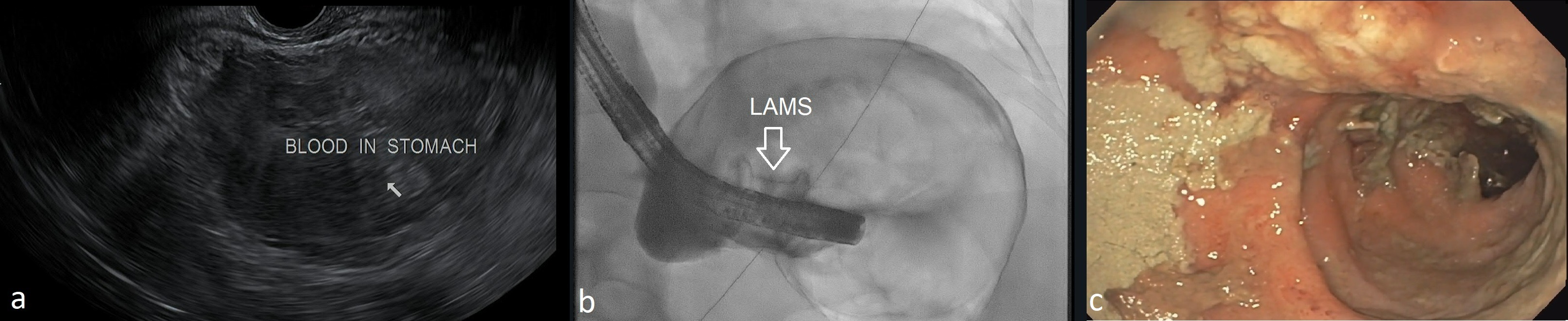
The patient’s hemoglobin dropped to a nadir of 5.7, and she was referred for upper endoscopic ultrasound which demonstrated a very large clot burden within the excluded stomach (Figure 1-a), and an ultrasound-guided gastrogastric lumen apposing metal stent (LAMS) was placed from the gastric pouch into the excluded stomach. The stent was successfully dilated and fixed with stay sutures (Figure1-b). A large burden of clot was subsequently removed from the excluded stomach and duodenum. A deep ulcer with active bleeding was localized to the posterior wall of the duodenum.
Bipolar cautery and epinephrine injection were used initially but failed to achieve hemostasis. Over-the-scope clip was considered but given the lack of having a mature gastrogastric fistula tract it was instead elected to use hemostatic powder application (figure 1-c). With this, complete hemostasis was achieved, and the LAMS stent was left in place for subsequent intervention(s) as needed.
The patient continued to pass melena for 3 days post procedure with stable Hb readings and follow up EGD showed no signs of active bleeding in the excluded stomach or duodenum. At 6 weeks, the LAMS was removed and the gastrogastric fistula tract was closed with argon plasma resurfacing and suture.
Discussion: Identification the source of UGIB in RYGB patients can be challenging. Accessing the excluded stomach should be considered early in the evaluation if the EGD shows no obvious source of bleeding or if other evaluation (such as angiogram) suggests a remnant stomach or duodenal source.
Disclosures:
Mohammad Alqaisieh, MD1, Karl Akiki, MD2, Tala Mahmoud, MD2, Andrew C. Storm, MD2. B0320 - Remnant Stomach Bleeding in Roux-en-Y Gastric Bypass Anatomy Managed by Transgastric Endoscopic Ultrasound-Guided Stenting and Hemostasis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Mayo Clinic, Dalton, GA; 2Mayo Clinic, Rochester, MN
Introduction: Upper GI bleeding identification and treatment is challenging in patients with Roux-en-Y gastric bypass (RYGB) due to their complex anatomy. Remnant stomach and duodenal bleeding in particular can be very challenging to reach and manage endoscopically due to the long length of the Roux and biliary limb.
Case Description/Methods: A 58-year-old female patient, who underwent gastric bypass in 2004, was diagnosed with fibular fracture and placed on NSAIDs 2 weeks before presenting to the hospital with melena and anemia. In addition to medical management of hypovolemic shock, the patient underwent upper endoscopy (EGD), colonoscopy, small bowel enteroscopy, and angiography followed by left gastric artery embolization all of which failed to localize or stop her bleeding.
The patient’s hemoglobin dropped to a nadir of 5.7, and she was referred for upper endoscopic ultrasound which demonstrated a very large clot burden within the excluded stomach (Figure 1-a), and an ultrasound-guided gastrogastric lumen apposing metal stent (LAMS) was placed from the gastric pouch into the excluded stomach. The stent was successfully dilated and fixed with stay sutures (Figure1-b). A large burden of clot was subsequently removed from the excluded stomach and duodenum. A deep ulcer with active bleeding was localized to the posterior wall of the duodenum.
Bipolar cautery and epinephrine injection were used initially but failed to achieve hemostasis. Over-the-scope clip was considered but given the lack of having a mature gastrogastric fistula tract it was instead elected to use hemostatic powder application (figure 1-c). With this, complete hemostasis was achieved, and the LAMS stent was left in place for subsequent intervention(s) as needed.
The patient continued to pass melena for 3 days post procedure with stable Hb readings and follow up EGD showed no signs of active bleeding in the excluded stomach or duodenum. At 6 weeks, the LAMS was removed and the gastrogastric fistula tract was closed with argon plasma resurfacing and suture.
Discussion: Identification the source of UGIB in RYGB patients can be challenging. Accessing the excluded stomach should be considered early in the evaluation if the EGD shows no obvious source of bleeding or if other evaluation (such as angiogram) suggests a remnant stomach or duodenal source.
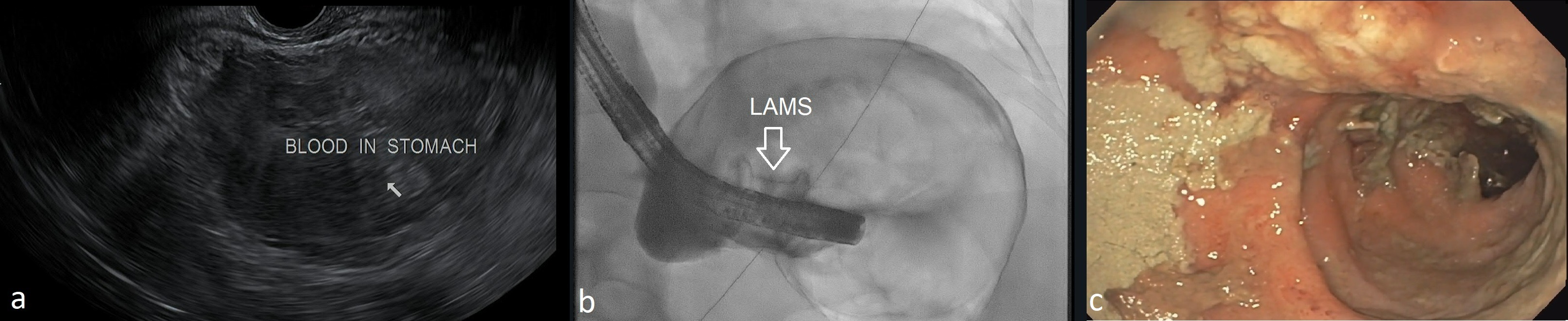
Figure: Figure 1: a- Endosonographic photo showing blood in the remnant stomach, b- Fluoroscopy showing proper placement and dilatation of the gastrogastric LAMS , c- Endoscopic photo showing complete hemostasis after hemostatic powder application.
Disclosures:
Mohammad Alqaisieh indicated no relevant financial relationships.
Karl Akiki indicated no relevant financial relationships.
Tala Mahmoud indicated no relevant financial relationships.
Andrew Storm: Apollo Endosurgery – Consultant. Apollo Endosurgery – Grant/Research Support. Boston Scientific – Grant/Research Support. Endo-TAGSS – Grant/Research Support. Enterasense – Consultant. ERBE – Consultant. GI Dynamics – Consultant. Olympus – Consultant.
Mohammad Alqaisieh, MD1, Karl Akiki, MD2, Tala Mahmoud, MD2, Andrew C. Storm, MD2. B0320 - Remnant Stomach Bleeding in Roux-en-Y Gastric Bypass Anatomy Managed by Transgastric Endoscopic Ultrasound-Guided Stenting and Hemostasis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

