Back

Poster Session B - Monday Morning
Category: GI Bleeding
B0333 - Don’t Get Fooled: Scurvy Can Mimic Portal Hypertensive Gastropathy Bleeding
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Hamza Ertugrul, MD
University of Missouri
Columbia, MO
Presenting Author(s)
Award: Presidential Poster Award
Hamza Ertugrul, MD1, Harleen K. Chela, MD2, Alp Kahveci, 1, Tahan Veysel, MD1, Ebubekir Daglilar, MD1
1University of Missouri, Columbia, MO; 2University of Missouri-Columbia, Columbia, MO
Introduction: Vitamin C deficiency, also known as scurvy, is a rare cause of significant mucosal bleeding that can easily be missed. It can manifest as diffuse hemorrhage with normal coagulation tests. We describe a case of refractory upper gastrointestinal (GI) bleeding from Vitamin C deficiency initially thought to be related to portal hypertensive gastropathy.
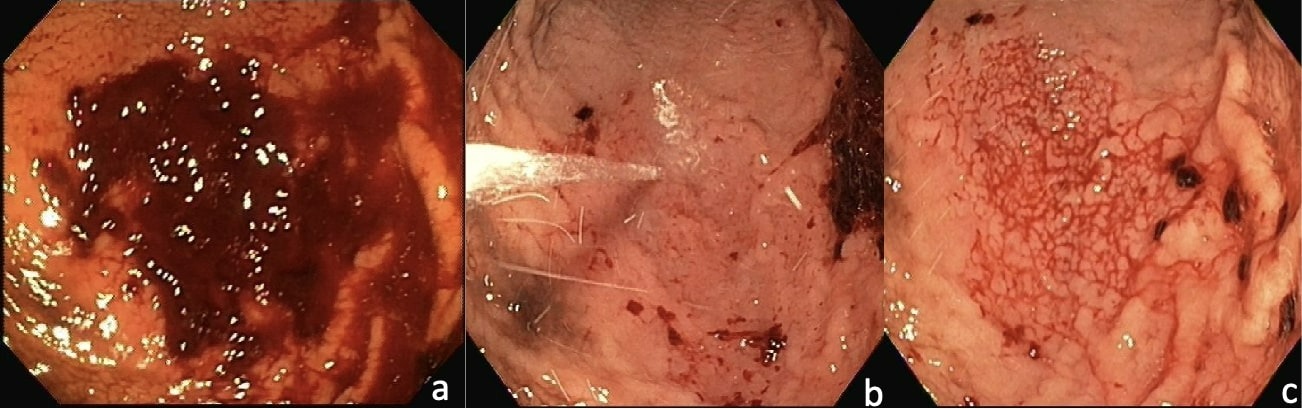
Case Description/Methods: A 56-year-old female with depression, BMI of 74kg/m2, and a recent admission for strangulated ventral hernia with small bowel resection presented to the emergency room with episodes of melena. Labs on admission were notable for Hgb 6.1g/dL, down from 11.2 on discharge, and an elevated BUN with normal creatinine, INR and platelets. CT scan showed mild splenomegaly and postsurgical changes of ventral hernia repair with no anastomotic leak or bleeding. Urgent EGD was performed demonstrating clots in the stomach which later removed. Diffuse hemorrhage from distal gastric body with rapid accumulation of blood following washing with water seen. Hemostasis was achieved with hemostatic powder spray. Next day, patient continued to have melena and required blood transfusions. Tagged RBC scan was performed to rule out additional sources of bleeding, demonstrated ongoing bleeding from distal gastric body. Repeat EGD was performed and area treated with argon plasma coagulation and hemostatic powder. Despite our efforts, patient continued to have slow bleeding and required a total of 17 units of blood.
Bleeding initially thought to be due to portal hypertensive gastropathy given risk factors for NASH, however, in the absence of additional clinical evidence beyond mild splenomegaly, underlying bleeding diathesis was suspected. Hematology was consulted. Duloxetine was discontinued due to possible platelet dysfunction. Hematological workup was normal including normal PFA-100, VWF, factor VIII, XIII, ECLT, fibrinogen, ECLT, D-Dimer. Notably, Vitamin C levels were found to be below < 0.1mg/dL. A diagnosis of scurvy was made and patient was initiated on high dose ascorbic acid. Within 24 hours of treatment, bleeding had resolved.
Discussion: Morbidly obese patients are predisposed to developing nutritional deficiencies. Vitamin C deficiency should be considered in the differential of severe refractory GI bleeding in post-surgical patients. Treatment is as simple as replacement of Vitamin C, with swift improvement expected.
Disclosures:
Hamza Ertugrul, MD1, Harleen K. Chela, MD2, Alp Kahveci, 1, Tahan Veysel, MD1, Ebubekir Daglilar, MD1. B0333 - Don’t Get Fooled: Scurvy Can Mimic Portal Hypertensive Gastropathy Bleeding, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Hamza Ertugrul, MD1, Harleen K. Chela, MD2, Alp Kahveci, 1, Tahan Veysel, MD1, Ebubekir Daglilar, MD1
1University of Missouri, Columbia, MO; 2University of Missouri-Columbia, Columbia, MO
Introduction: Vitamin C deficiency, also known as scurvy, is a rare cause of significant mucosal bleeding that can easily be missed. It can manifest as diffuse hemorrhage with normal coagulation tests. We describe a case of refractory upper gastrointestinal (GI) bleeding from Vitamin C deficiency initially thought to be related to portal hypertensive gastropathy.
Case Description/Methods: A 56-year-old female with depression, BMI of 74kg/m2, and a recent admission for strangulated ventral hernia with small bowel resection presented to the emergency room with episodes of melena. Labs on admission were notable for Hgb 6.1g/dL, down from 11.2 on discharge, and an elevated BUN with normal creatinine, INR and platelets. CT scan showed mild splenomegaly and postsurgical changes of ventral hernia repair with no anastomotic leak or bleeding. Urgent EGD was performed demonstrating clots in the stomach which later removed. Diffuse hemorrhage from distal gastric body with rapid accumulation of blood following washing with water seen. Hemostasis was achieved with hemostatic powder spray. Next day, patient continued to have melena and required blood transfusions. Tagged RBC scan was performed to rule out additional sources of bleeding, demonstrated ongoing bleeding from distal gastric body. Repeat EGD was performed and area treated with argon plasma coagulation and hemostatic powder. Despite our efforts, patient continued to have slow bleeding and required a total of 17 units of blood.
Bleeding initially thought to be due to portal hypertensive gastropathy given risk factors for NASH, however, in the absence of additional clinical evidence beyond mild splenomegaly, underlying bleeding diathesis was suspected. Hematology was consulted. Duloxetine was discontinued due to possible platelet dysfunction. Hematological workup was normal including normal PFA-100, VWF, factor VIII, XIII, ECLT, fibrinogen, ECLT, D-Dimer. Notably, Vitamin C levels were found to be below < 0.1mg/dL. A diagnosis of scurvy was made and patient was initiated on high dose ascorbic acid. Within 24 hours of treatment, bleeding had resolved.
Discussion: Morbidly obese patients are predisposed to developing nutritional deficiencies. Vitamin C deficiency should be considered in the differential of severe refractory GI bleeding in post-surgical patients. Treatment is as simple as replacement of Vitamin C, with swift improvement expected.
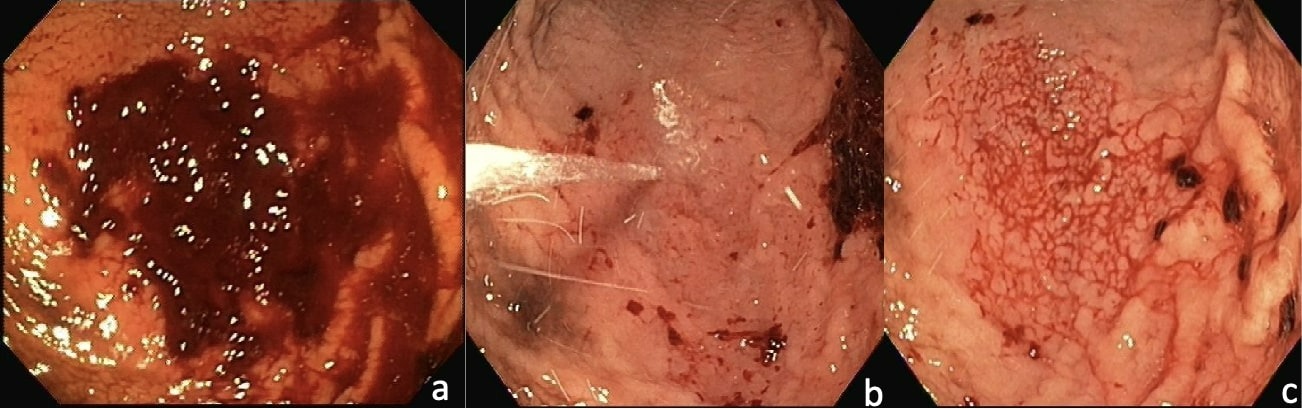
Figure: Figure a: residual clot noted in the stomach.
Figure b: Distal gastric body being washed with water.
Figure c: Rapid re-accumulation of hemorrhagic areas with oozing noted.
Figure b: Distal gastric body being washed with water.
Figure c: Rapid re-accumulation of hemorrhagic areas with oozing noted.
Disclosures:
Hamza Ertugrul indicated no relevant financial relationships.
Harleen Chela indicated no relevant financial relationships.
Alp Kahveci indicated no relevant financial relationships.
Tahan Veysel indicated no relevant financial relationships.
Tahan Veysel — NO DISCLOSURE DATA.
Ebubekir Daglilar indicated no relevant financial relationships.
Hamza Ertugrul, MD1, Harleen K. Chela, MD2, Alp Kahveci, 1, Tahan Veysel, MD1, Ebubekir Daglilar, MD1. B0333 - Don’t Get Fooled: Scurvy Can Mimic Portal Hypertensive Gastropathy Bleeding, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

