Back

Poster Session E - Tuesday Afternoon
Category: Biliary/Pancreas
E0083 - An Unusual Location of Pseudoaneurysm in the Setting of Acute Severe Pancreatitis
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Romy Chamoun, MD
Lankenau Medical Center
Wynnewood, PA
Presenting Author(s)
Romy Chamoun, MD1, Rachael Schneider, DO2, Bryan Stone, DO1, Roy Taoutel, MD1
1Lankenau Medical Center, Wynnewood, PA; 2Main Line Health - Lankenau Hospital, Wynnewood, PA
Introduction: Acute pancreatitis (AP) is one of the most common gastroenterological causes of hospital admissions. The mortality rate of AP is around 10% despite medical advancements. Around 4-17% of cases of acute pancreatitis are complicated by the formation of pseudoaneurysms. The most commonly involved arteries are splenic artery (60-65%), gastroduodenal (20-25%), pancreaticoduodenal (10-15%), hepatic (5-10%) and left gastric arteries (2-5%). We present a case of superior mesenteric artery (SMA) pseudoaneurysm secondary to acute severe pancreatitis.
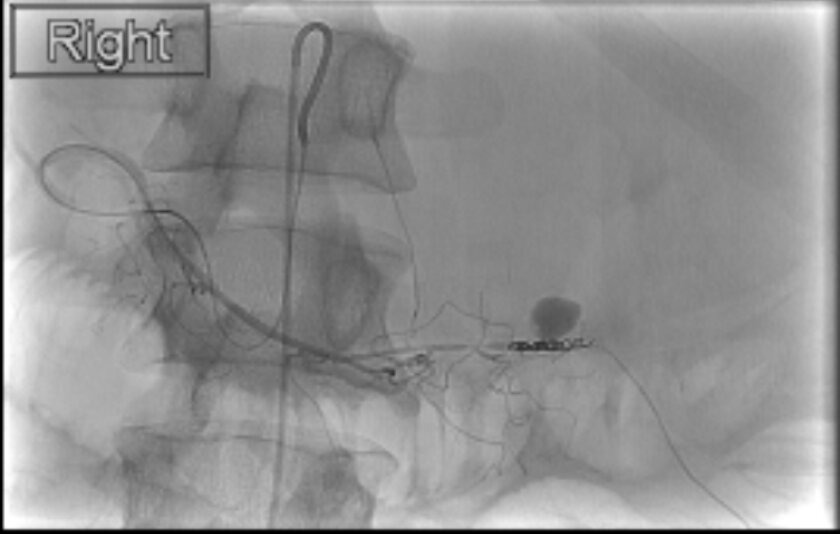
Case Description/Methods: A 33-year-old male patient with a past medical history of alcohol abuse presented to the hospital for abdominal pain after an alcohol binge. He was found to have significant acute kidney injury, metabolic acidosis, and leukocytosis to 24 K/uL. CT showed acute pancreatitis and a large peripancreatic collection consistent with hemorrhage with posterolateral extension into the left iliopsoas space. He was found to have staphylococcus aureus bacteremia thus he was initially treated with fluid resuscitation and cefazolin. Several days into the admission he had an episode of hemodynamic instability with a CT showing a 7 mm pseudoaneurysm seen within the collection with active contrast extravasation. His hemoglobin dropped 2g during this episode requiring pRBC transfusion. He underwent IR coil embolization of the middle colic branch of the SMA. During a subsequent admission, he had worsening abdominal pain and distension with radiographic evidence of enlarging collections so a drain was placed into the peripancreatic collection by IR with improvement in symptoms.
Discussion: Pseudoaneurysm formation is an uncommon but life-threatening complication of pancreatitis. Pancreatic enzymes released in the setting of pancreatic inflammation leak into vessel walls causing destruction. The majority develop in the splenic artery given the proximity to the pancreas. Those in the SMA account for just 5% of cases. CT angiography is the best diagnostic modality for assessing pseudoaneurysm arterial bleeding. Treatment in the past was primarily surgical but with endovascular advancements, embolization with coils or glue is now first line. However, many patients may still require surgery if embolization fails or if hemodynamically unstable. Despite the rarity of pseudoaneurysm formation, it is important to have knowledge of the appropriate diagnostic workup and treatment given the potentially high mortality rate.
Disclosures:
Romy Chamoun, MD1, Rachael Schneider, DO2, Bryan Stone, DO1, Roy Taoutel, MD1. E0083 - An Unusual Location of Pseudoaneurysm in the Setting of Acute Severe Pancreatitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Lankenau Medical Center, Wynnewood, PA; 2Main Line Health - Lankenau Hospital, Wynnewood, PA
Introduction: Acute pancreatitis (AP) is one of the most common gastroenterological causes of hospital admissions. The mortality rate of AP is around 10% despite medical advancements. Around 4-17% of cases of acute pancreatitis are complicated by the formation of pseudoaneurysms. The most commonly involved arteries are splenic artery (60-65%), gastroduodenal (20-25%), pancreaticoduodenal (10-15%), hepatic (5-10%) and left gastric arteries (2-5%). We present a case of superior mesenteric artery (SMA) pseudoaneurysm secondary to acute severe pancreatitis.
Case Description/Methods: A 33-year-old male patient with a past medical history of alcohol abuse presented to the hospital for abdominal pain after an alcohol binge. He was found to have significant acute kidney injury, metabolic acidosis, and leukocytosis to 24 K/uL. CT showed acute pancreatitis and a large peripancreatic collection consistent with hemorrhage with posterolateral extension into the left iliopsoas space. He was found to have staphylococcus aureus bacteremia thus he was initially treated with fluid resuscitation and cefazolin. Several days into the admission he had an episode of hemodynamic instability with a CT showing a 7 mm pseudoaneurysm seen within the collection with active contrast extravasation. His hemoglobin dropped 2g during this episode requiring pRBC transfusion. He underwent IR coil embolization of the middle colic branch of the SMA. During a subsequent admission, he had worsening abdominal pain and distension with radiographic evidence of enlarging collections so a drain was placed into the peripancreatic collection by IR with improvement in symptoms.
Discussion: Pseudoaneurysm formation is an uncommon but life-threatening complication of pancreatitis. Pancreatic enzymes released in the setting of pancreatic inflammation leak into vessel walls causing destruction. The majority develop in the splenic artery given the proximity to the pancreas. Those in the SMA account for just 5% of cases. CT angiography is the best diagnostic modality for assessing pseudoaneurysm arterial bleeding. Treatment in the past was primarily surgical but with endovascular advancements, embolization with coils or glue is now first line. However, many patients may still require surgery if embolization fails or if hemodynamically unstable. Despite the rarity of pseudoaneurysm formation, it is important to have knowledge of the appropriate diagnostic workup and treatment given the potentially high mortality rate.
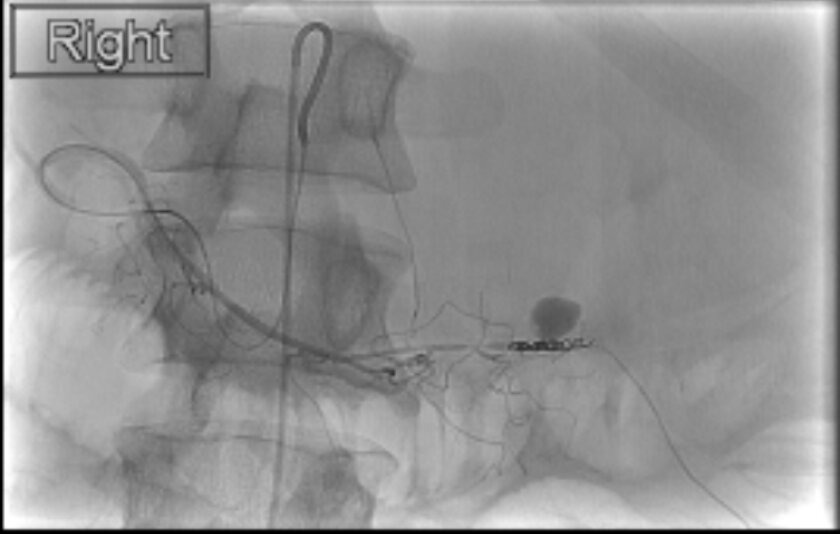
Figure: IR coil embolization of the middle colic branch of the SMA
Disclosures:
Romy Chamoun indicated no relevant financial relationships.
Rachael Schneider indicated no relevant financial relationships.
Bryan Stone indicated no relevant financial relationships.
Roy Taoutel indicated no relevant financial relationships.
Romy Chamoun, MD1, Rachael Schneider, DO2, Bryan Stone, DO1, Roy Taoutel, MD1. E0083 - An Unusual Location of Pseudoaneurysm in the Setting of Acute Severe Pancreatitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
