Back

Poster Session B - Monday Morning
Category: Biliary/Pancreas
B0081 - Pancreatitis, Panniculitis and Polyarthralgia Syndrome: A Rare Complication of Pancreatic Pathology
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Parth M. Patel, MD
Henry Ford Jackson
Jackson, MI
Presenting Author(s)
Parth M. Patel, MD, Harjinder Singh, MD, Shamik Parikh, MD, Hassan Zreik, MD, Vivek Kak, MD
Henry Ford Jackson, Jackson, MI
Introduction: Pancreatitis, panniculitis, and polyarthritis (PPP) syndrome is a rare syndrome consisting of multiorgan extra-pancreatic manifestations of pancreatitis due to high serum lipase levels. Patients can often have little to no abdominal symptoms. The syndrome can also mimic infectious etiologies leading to misdiagnosis, mistreatment, and the possibility of deterioration.
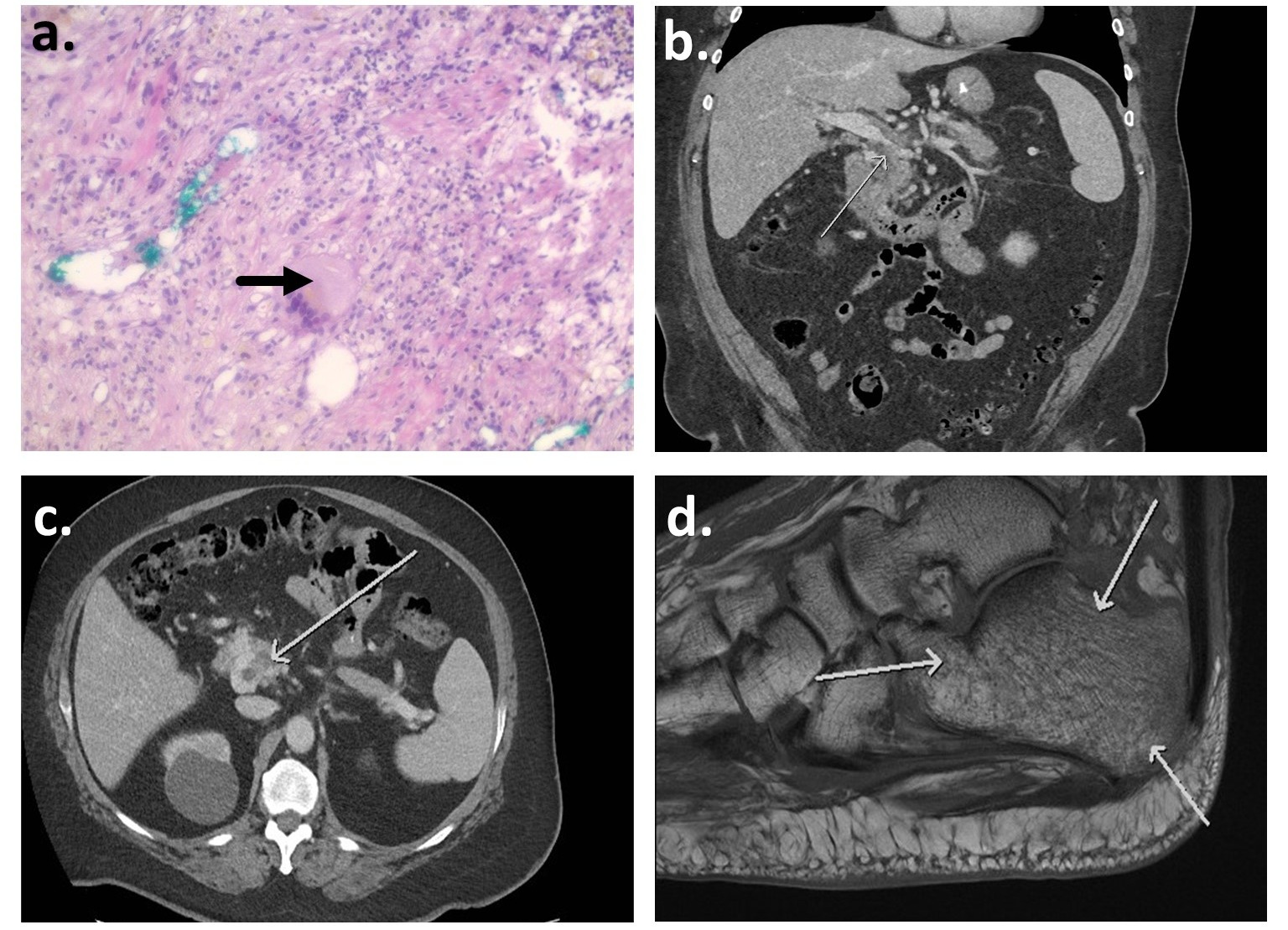
Case Description/Methods: A 64-year-old male with a history of alcohol abuse presented with painful nodular purulent lesions in his legs and bilateral joint pain in his hips and shoulders. NSAIDs and glucocorticoids did not provide relief. He was initially diagnosed with erythema nodosum. The patient had an elevated Erythrocyte Sedimentation Rate of 75 mm/h, C-reactive protein of 5.7 mg/dL, slightly elevated transaminases, and elevated Lipase of 2328 U/L. A basic metabolic profile and complete blood count were unremarkable. A computed tomography scan of the abdomen showed acute pancreatitis with peripancreatic inflammatory changes. It also showed partial occlusion thrombosis of the portal and superior mesenteric veins. Notably, the patient did not have any abdominal pain on presentation. MRI of the left calcaneus showed bone edema suggesting radiographic evidence of osteomyelitis. The patient was treated with a prolonged course of broad-spectrum antibiotics without improvement. A biopsy of the panniculitis lesions showed lobular panniculitis and ghost cells which were pathognomonic for pancreatic panniculitis. Hence, the cause of panniculitis and bone necrosis was thought to be due to the intravascular leakage of lipase due to PPP syndrome. The patient’s polyarthralgia was described due to the deposition of free fatty acids in joints following fat autodigestion.
Discussion: After the diagnosis of PPP syndrome, the patient was largely asymptomatic. This case highlights the importance of bone biopsy in diagnosing osteomyelitis. Reactive changes in bone on imaging could be seen in other non-infectious pathologies such as PPP syndrome, as highlighted in this case. The delayed diagnosis led to poor antibiotic stewardship and delay in treatment. This case also demonstrates the importance of a multidisciplinary team in identifying and managing a rare disease.
Disclosures:
Parth M. Patel, MD, Harjinder Singh, MD, Shamik Parikh, MD, Hassan Zreik, MD, Vivek Kak, MD. B0081 - Pancreatitis, Panniculitis and Polyarthralgia Syndrome: A Rare Complication of Pancreatic Pathology, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Henry Ford Jackson, Jackson, MI
Introduction: Pancreatitis, panniculitis, and polyarthritis (PPP) syndrome is a rare syndrome consisting of multiorgan extra-pancreatic manifestations of pancreatitis due to high serum lipase levels. Patients can often have little to no abdominal symptoms. The syndrome can also mimic infectious etiologies leading to misdiagnosis, mistreatment, and the possibility of deterioration.
Case Description/Methods: A 64-year-old male with a history of alcohol abuse presented with painful nodular purulent lesions in his legs and bilateral joint pain in his hips and shoulders. NSAIDs and glucocorticoids did not provide relief. He was initially diagnosed with erythema nodosum. The patient had an elevated Erythrocyte Sedimentation Rate of 75 mm/h, C-reactive protein of 5.7 mg/dL, slightly elevated transaminases, and elevated Lipase of 2328 U/L. A basic metabolic profile and complete blood count were unremarkable. A computed tomography scan of the abdomen showed acute pancreatitis with peripancreatic inflammatory changes. It also showed partial occlusion thrombosis of the portal and superior mesenteric veins. Notably, the patient did not have any abdominal pain on presentation. MRI of the left calcaneus showed bone edema suggesting radiographic evidence of osteomyelitis. The patient was treated with a prolonged course of broad-spectrum antibiotics without improvement. A biopsy of the panniculitis lesions showed lobular panniculitis and ghost cells which were pathognomonic for pancreatic panniculitis. Hence, the cause of panniculitis and bone necrosis was thought to be due to the intravascular leakage of lipase due to PPP syndrome. The patient’s polyarthralgia was described due to the deposition of free fatty acids in joints following fat autodigestion.
Discussion: After the diagnosis of PPP syndrome, the patient was largely asymptomatic. This case highlights the importance of bone biopsy in diagnosing osteomyelitis. Reactive changes in bone on imaging could be seen in other non-infectious pathologies such as PPP syndrome, as highlighted in this case. The delayed diagnosis led to poor antibiotic stewardship and delay in treatment. This case also demonstrates the importance of a multidisciplinary team in identifying and managing a rare disease.
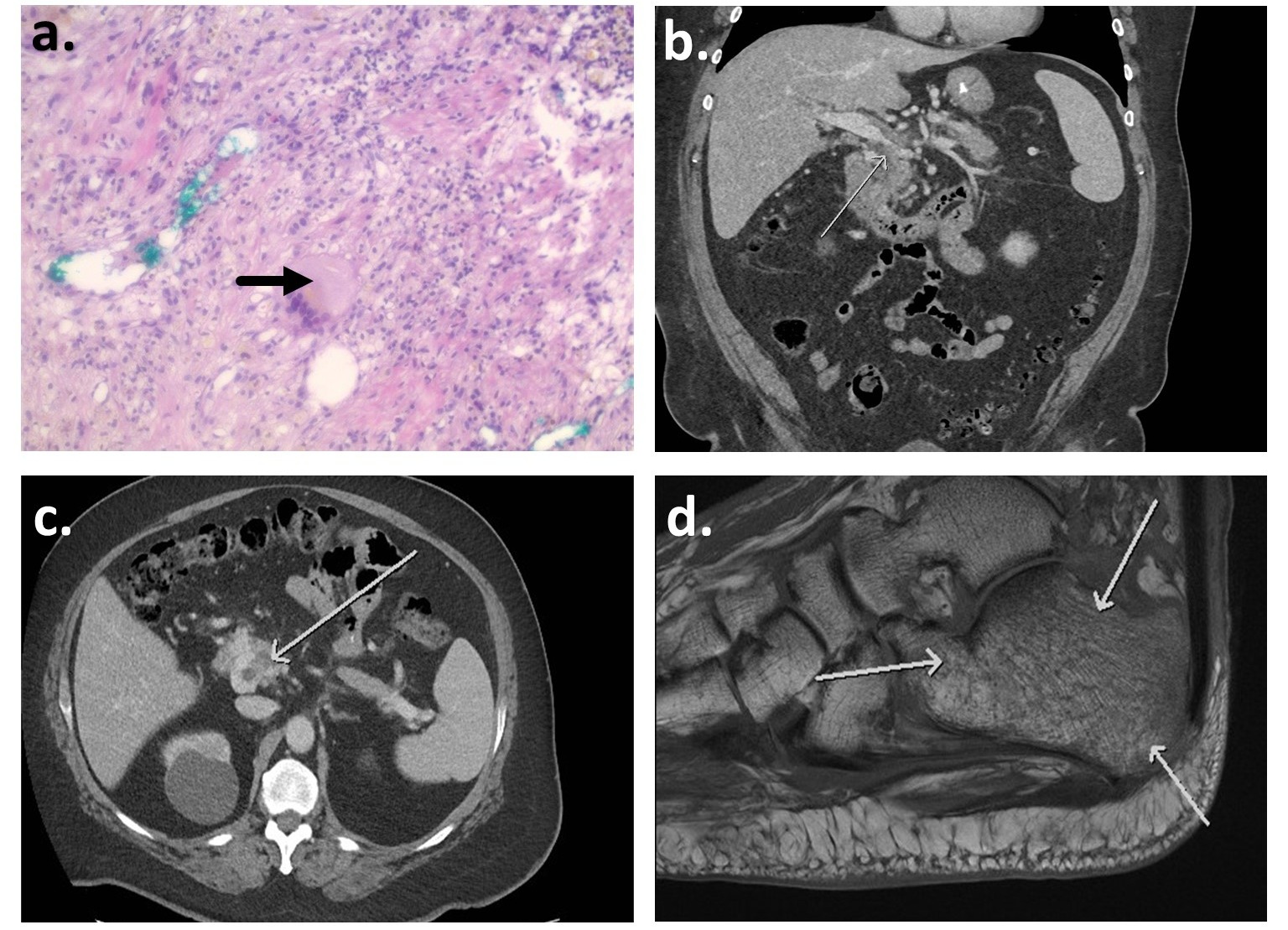
Figure: Figure 1: a. H&E stain of panniculitis lesion biopsy showing ghost cell (arrow) with a background of inflammation suggesting pancreatic panniculitis b. Partial thrombosis of portal vein (arrow) on CT of abdomen (coronal view) c. Partial thrombosis of superior mesenteric vein (arrow) in transverse view of CT abdomen d. Reactive bone changes on MRI of left foot (arrows)
Disclosures:
Parth Patel indicated no relevant financial relationships.
Harjinder Singh indicated no relevant financial relationships.
Shamik Parikh indicated no relevant financial relationships.
Hassan Zreik indicated no relevant financial relationships.
Vivek Kak indicated no relevant financial relationships.
Parth M. Patel, MD, Harjinder Singh, MD, Shamik Parikh, MD, Hassan Zreik, MD, Vivek Kak, MD. B0081 - Pancreatitis, Panniculitis and Polyarthralgia Syndrome: A Rare Complication of Pancreatic Pathology, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
