Back

Poster Session C - Monday Afternoon
Category: GI Bleeding
C0340 - Splenic Vein Stenting and Endovascular Embolization for Bleeding Isolated Gastric Varices: A Spleen-Sparing Solution
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Steve Obanor, MD
Maimonides Medical Center
Brooklyn, NY
Presenting Author(s)
Steve Obanor, MD1, Kunzah A. Syed, DO2, Avleen Kaur, MD1, Kadirawel Iswara, MD, FACG1
1Maimonides Medical Center, Brooklyn, NY; 2Memorial Sloan Kettering Cancer Center, Manhattan, NY
Introduction: Splenic vein thrombosis (SVT) typically occurs in the context of pancreatic diseases and leads to sinistral portal hypertension. Splenectomy is the treatment of choice and curative for bleeding from resultant isolated gastric varices (IGV). We report a unique approach to the management of gastric variceal bleeding secondary to SVT in the absence of malignancy or chronic pancreatitis. Hemostasis was achieved by recanalization of the splenic vein (SV) and subsequent embolization of gastric varices.
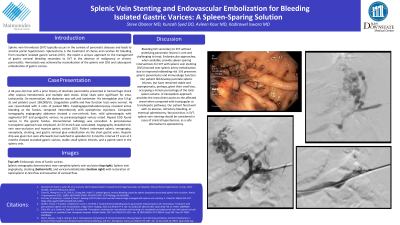
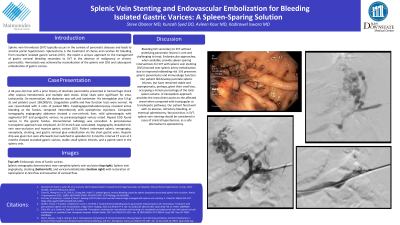
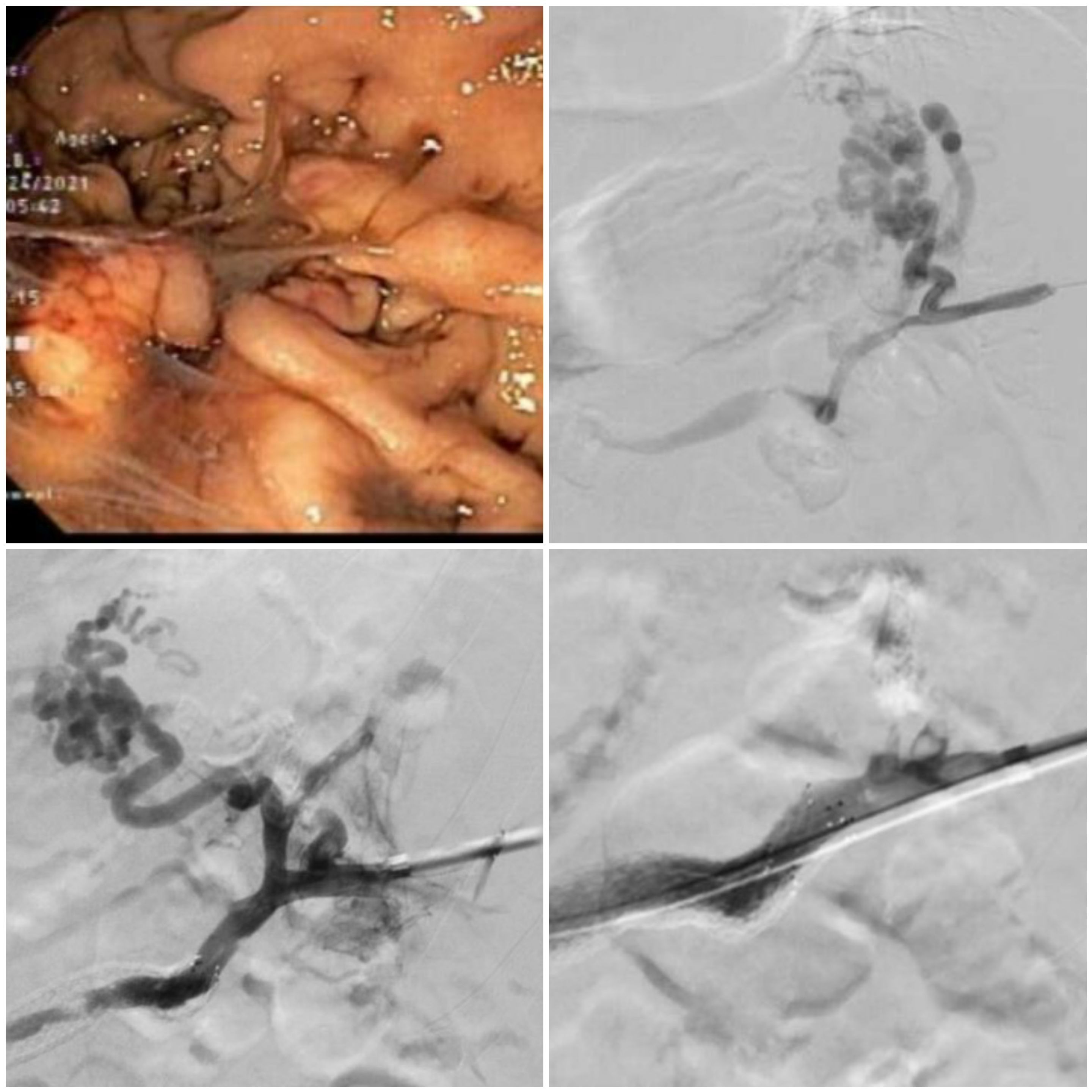
Case Description/Methods: A 43-year-old man with a prior history of alcoholic pancreatitis presented in hemorrhagic shock after copious hematemesis and multiple dark stools. Initial vitals were significant for sinus tachycardia. On examination, the abdomen was soft and nontender. His hemoglobin was 5.9 g/dL and platelet count 269,000/UL. Coagulation profile and liver function tests were normal. He was resuscitated with 3 units of packed RBCs. Esophagogastroduodenoscopy (EGD) revealed active bleeding at the fundus, tempered intermittently with epinephrine injections. Computed tomography (CT) angiography abdomen showed mild splenomegaly with segmental SVT and perigastric varices. Repeat EGD found varices in the gastric fundus. Interventional radiology was consulted. A percutaneous transsplenic approach was employed. An SV branch was cannulated. Angiography revealed mid-vein near-occlusion and massive gastric varices (GV). He underwent venoplasty, stenting, venography, and gastric variceal glue embolization. Heparin drip was given but soon switched to apixaban for 6 months. CT scan confirmed new splenic infarcts and a stent in the patent SV. At 3 months, CT abdomen showed an occluded GV and stent patency.
Discussion: Bleeding IGV secondary to SVT without underlying pancreatic lesions is rare and challenging to treat. Endovascular approaches, when available, provide spleen-sparing interventions for SVT with splenic vein stenting (SVS) favored over splenic artery embolization (SAE) due to improved rebleeding risk. SVS preserves splenic parenchyma and immunologic function. A transsplenic approach provides the most direct access to the affected vessel when compared with transjugular or transhepatic pathways. Our patient fared well with no abscess, refractory bleeding, or eventual splenectomy. We posit that in SVT, splenic vein stenting should be considered in cases of sinistral hypertension, as a safe alternative to splenectomy.
Disclosures:
Steve Obanor, MD1, Kunzah A. Syed, DO2, Avleen Kaur, MD1, Kadirawel Iswara, MD, FACG1. C0340 - Splenic Vein Stenting and Endovascular Embolization for Bleeding Isolated Gastric Varices: A Spleen-Sparing Solution, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Maimonides Medical Center, Brooklyn, NY; 2Memorial Sloan Kettering Cancer Center, Manhattan, NY
Introduction: Splenic vein thrombosis (SVT) typically occurs in the context of pancreatic diseases and leads to sinistral portal hypertension. Splenectomy is the treatment of choice and curative for bleeding from resultant isolated gastric varices (IGV). We report a unique approach to the management of gastric variceal bleeding secondary to SVT in the absence of malignancy or chronic pancreatitis. Hemostasis was achieved by recanalization of the splenic vein (SV) and subsequent embolization of gastric varices.
Case Description/Methods: A 43-year-old man with a prior history of alcoholic pancreatitis presented in hemorrhagic shock after copious hematemesis and multiple dark stools. Initial vitals were significant for sinus tachycardia. On examination, the abdomen was soft and nontender. His hemoglobin was 5.9 g/dL and platelet count 269,000/UL. Coagulation profile and liver function tests were normal. He was resuscitated with 3 units of packed RBCs. Esophagogastroduodenoscopy (EGD) revealed active bleeding at the fundus, tempered intermittently with epinephrine injections. Computed tomography (CT) angiography abdomen showed mild splenomegaly with segmental SVT and perigastric varices. Repeat EGD found varices in the gastric fundus. Interventional radiology was consulted. A percutaneous transsplenic approach was employed. An SV branch was cannulated. Angiography revealed mid-vein near-occlusion and massive gastric varices (GV). He underwent venoplasty, stenting, venography, and gastric variceal glue embolization. Heparin drip was given but soon switched to apixaban for 6 months. CT scan confirmed new splenic infarcts and a stent in the patent SV. At 3 months, CT abdomen showed an occluded GV and stent patency.
Discussion: Bleeding IGV secondary to SVT without underlying pancreatic lesions is rare and challenging to treat. Endovascular approaches, when available, provide spleen-sparing interventions for SVT with splenic vein stenting (SVS) favored over splenic artery embolization (SAE) due to improved rebleeding risk. SVS preserves splenic parenchyma and immunologic function. A transsplenic approach provides the most direct access to the affected vessel when compared with transjugular or transhepatic pathways. Our patient fared well with no abscess, refractory bleeding, or eventual splenectomy. We posit that in SVT, splenic vein stenting should be considered in cases of sinistral hypertension, as a safe alternative to splenectomy.
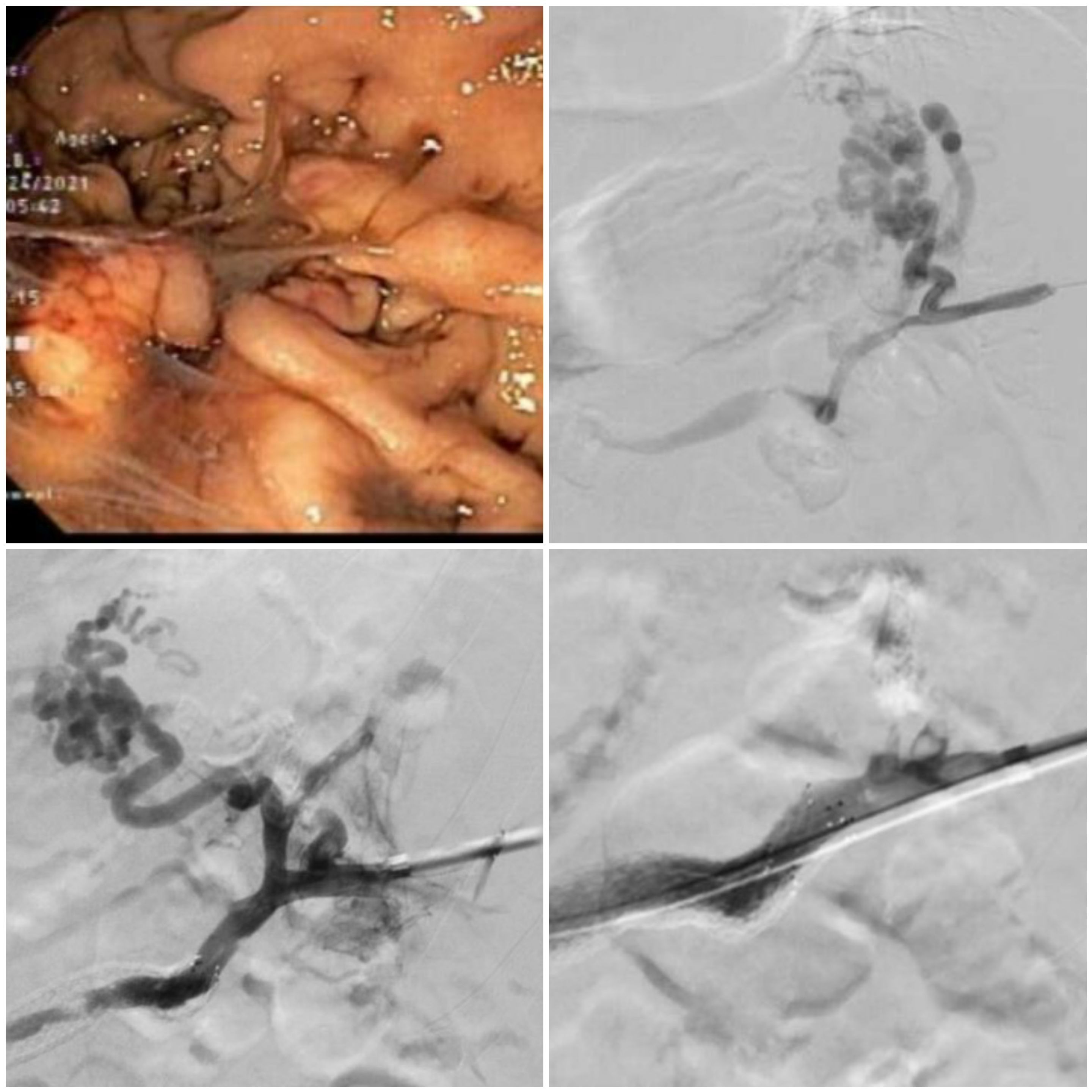
Figure: From left to right and top to bottom: Endoscopic view of fundal varices. Splenoportography showing stenosed splenic vein and perigastric varices. Flow post stenting. Flow post embolization.
Disclosures:
Steve Obanor indicated no relevant financial relationships.
Kunzah Syed indicated no relevant financial relationships.
Avleen Kaur indicated no relevant financial relationships.
Kadirawel Iswara indicated no relevant financial relationships.
Steve Obanor, MD1, Kunzah A. Syed, DO2, Avleen Kaur, MD1, Kadirawel Iswara, MD, FACG1. C0340 - Splenic Vein Stenting and Endovascular Embolization for Bleeding Isolated Gastric Varices: A Spleen-Sparing Solution, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
