Back

Poster Session E - Tuesday Afternoon
Category: Colon
E0113 - A Case of Isolated Colonic MALT Lymphoma and Synchronous Celiac Disease
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Ted A. Spiewak, DO
San Antonio Military Medical Center
Ft Sam Houston, TX
Presenting Author(s)
Award: Presidential Poster Award
Ted A. Spiewak, DO1, Dianna Chormanski, MD2, Geoffrey A. Bader, MD2, Samuel C. Owen, MD1
1San Antonio Military Medical Center, Fort Sam Houston, TX; 2Brooke Army Medical Center, Fort Sam Houston, TX
Introduction: Extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue (MALT lymphoma) is uncommon, accounting for 5% of all non-Hodgkin lymphoma (NHL). The most common site is the stomach with isolated colonic involvement comprising only 2.5% of all MALT lymphomas and less than 0.5% of all colon cancers. Up to 50% of cases are asymptomatic with a variable endoscopic appearance (polypoidal, ulcerative or mass-like) and there is a lack of clear guidance on management. While gastric MALT lymphomas are strongly linked to active Helicobacter pylori (H. pylori) infection they have also been associated with autoimmune diseases such as celiac disease (CD); a link that is uncertain with the colonic variety.
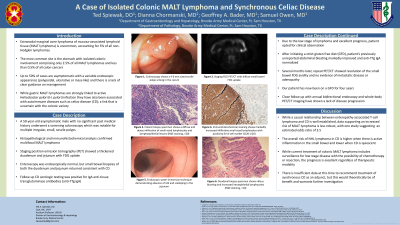
Case Description/Methods: A 50-year-old male underwent a screening colonoscopy notable for lymphoid aggregates and multiple irregular, small, sessile polyps. Histopathological and immunohistochemical analysis confirmed multifocal stage I MALT lymphoma. Positron emission tomography showed FDG uptake in a thickened duodenum and jejunum without corresponding findings on subsequent enteroscopy. Gastric biopsies were negative for H. pylori but small bowel biopsies were consistent with CD which was confirmed with elevated serum IgA anti-tissue transglutaminase antibodies (anti-TTg IgA). Neither radiation therapy nor surgery were pursued due to the extent of disease, the significant expected morbidly, and the low stage of the lymphoma. After initiating a gluten free diet his anti-TTg IgA normalized and the small bowel FDG avidity resolved. He had no metastatic disease and serial endoscopies have allowed resection of additional lesions.
Discussion: While a causal relationship between enteropathy-associated T-cell lymphoma and CD is well established, data supporting an increased risk of MALT lymphoma is less robust, but present in the literature with an estimated odds ratio in one study of 3.5. The overall risk of NHL lymphoma in CD is higher when there is active inflammation in the small bowel and lower when CD is quiescent. While current treatment of colonic MALT lymphoma includes surveillance for low stage disease with the possibility of chemotherapy or resection, the prognosis is excellent regardless of therapeutic modality. There is insufficient data at this time to recommend treatment of synchronous CD as an adjunct, but this would theoretically be of benefit and warrants further investigation.

Disclosures:
Ted A. Spiewak, DO1, Dianna Chormanski, MD2, Geoffrey A. Bader, MD2, Samuel C. Owen, MD1. E0113 - A Case of Isolated Colonic MALT Lymphoma and Synchronous Celiac Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Ted A. Spiewak, DO1, Dianna Chormanski, MD2, Geoffrey A. Bader, MD2, Samuel C. Owen, MD1
1San Antonio Military Medical Center, Fort Sam Houston, TX; 2Brooke Army Medical Center, Fort Sam Houston, TX
Introduction: Extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue (MALT lymphoma) is uncommon, accounting for 5% of all non-Hodgkin lymphoma (NHL). The most common site is the stomach with isolated colonic involvement comprising only 2.5% of all MALT lymphomas and less than 0.5% of all colon cancers. Up to 50% of cases are asymptomatic with a variable endoscopic appearance (polypoidal, ulcerative or mass-like) and there is a lack of clear guidance on management. While gastric MALT lymphomas are strongly linked to active Helicobacter pylori (H. pylori) infection they have also been associated with autoimmune diseases such as celiac disease (CD); a link that is uncertain with the colonic variety.
Case Description/Methods: A 50-year-old male underwent a screening colonoscopy notable for lymphoid aggregates and multiple irregular, small, sessile polyps. Histopathological and immunohistochemical analysis confirmed multifocal stage I MALT lymphoma. Positron emission tomography showed FDG uptake in a thickened duodenum and jejunum without corresponding findings on subsequent enteroscopy. Gastric biopsies were negative for H. pylori but small bowel biopsies were consistent with CD which was confirmed with elevated serum IgA anti-tissue transglutaminase antibodies (anti-TTg IgA). Neither radiation therapy nor surgery were pursued due to the extent of disease, the significant expected morbidly, and the low stage of the lymphoma. After initiating a gluten free diet his anti-TTg IgA normalized and the small bowel FDG avidity resolved. He had no metastatic disease and serial endoscopies have allowed resection of additional lesions.
Discussion: While a causal relationship between enteropathy-associated T-cell lymphoma and CD is well established, data supporting an increased risk of MALT lymphoma is less robust, but present in the literature with an estimated odds ratio in one study of 3.5. The overall risk of NHL lymphoma in CD is higher when there is active inflammation in the small bowel and lower when CD is quiescent. While current treatment of colonic MALT lymphoma includes surveillance for low stage disease with the possibility of chemotherapy or resection, the prognosis is excellent regardless of therapeutic modality. There is insufficient data at this time to recommend treatment of synchronous CD as an adjunct, but this would theoretically be of benefit and warrants further investigation.

Figure: Figure 1. Macro- and microscopic findings. (A) Colonoscopy shows a 4-6 mm sized sessile polyp arising in the cecum. (B) Endoscopic biopsy specimen shows a diffuse and dense infiltration of small-sized lymphocytes and lymphoepithelial lesions in the colonic mucosa (H&E staining, ×20). (C) Immunohistochemical staining shows markedly increased infiltrative small-sized lymphocytes with positivity for B-cell marker CD20 (×20).
Disclosures:
Ted Spiewak indicated no relevant financial relationships.
Dianna Chormanski indicated no relevant financial relationships.
Geoffrey Bader indicated no relevant financial relationships.
Samuel Owen indicated no relevant financial relationships.
Ted A. Spiewak, DO1, Dianna Chormanski, MD2, Geoffrey A. Bader, MD2, Samuel C. Owen, MD1. E0113 - A Case of Isolated Colonic MALT Lymphoma and Synchronous Celiac Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

