Back

Poster Session D - Tuesday Morning
Category: Stomach
D0715 - Synchronous Gastroesophageal Junction and Gastric Adenocarcinoma in an Otherwise Healthy Male
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Aireen Agulto, MD
University of Missouri Health Care
Columbia, MO
Presenting Author(s)
Aireen Agulto, MD1, Harleen K. Chela, MD2, Ghassan Hammoud, MD, MPH3
1University of Missouri Health Care, Columbia, MO; 2University of Missouri-Columbia, Columbia, MO; 3University of Missouri Health Care, Columbia, MO
Introduction: The incidence of multiple primary carcinomas (MPCs) is increasing but remains a rare diagnosis. MPCs are two or more unrelated cancers in one patient. The development of MPCs is theorized to be related to unhealthy lifestyles and genetic susceptibility. We present a previously healthy male without family history of GI malignancy diagnosed with synchronous gastroesophageal junction (GEJ) and gastric adenocarcinoma.
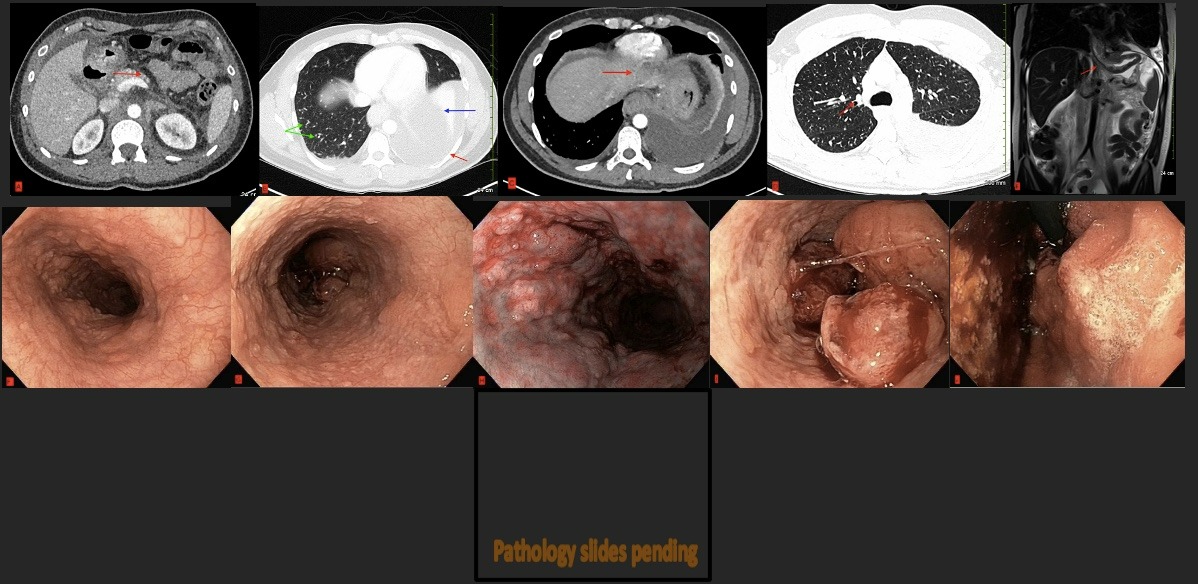
Case Description/Methods: A 41-year-old male without prior medical history presented with recent onset solid food dysphagia associated with worsening abdominal pain, weight loss, and dyspnea for 5 months. He denied alcohol or tobacco use, or family history of malignancy. Labs showed normal CEA and CA 19-9, and Computed Tomography (CT) of the chest and abdomen revealed bilateral pleural effusion with left lung collapse, numerous pulmonary nodules and enlarged mediastinal and abdominal lymph nodes (Figure A-B). There was a circumferential esophageal thickening at the GEJ and a concern for interstitial edematous pancreatitis (Figure C-D). Magnetic Resonance Imaging (MRI) of the abdomen revealed mesenteric nodularity concerning for peritoneal carcinomatosis and diffuse gastric wall and GEJ thickening concerning for malignancy (Figure E). His QuantiFERON-TB Gold (QFT) was positive, but AFB smears and PCR test were negative, consistent with latent TB. Upper GI endoscopy revealed extensive nodularity of the esophageal and gastric mucosa with a large ulcerated GEJ mass (Figure F-J). Gastric and esophageal biopsies revealed invasive adenocarcinoma with a differential expression of p53 staining, extensive mucinous features but without signet ring cells. Pleural and peritoneal fluid cytology were consistent with metastatic adenocarcinoma of primary GI origin. His hospital course was complicated by recurrent pleural effusions, pulmonary embolism and upper gastrointestinal bleeding. Patient was followed with oncology for chemoradiation therapy for advanced unresectable gastric and GEJ adenocarcinoma with distant metastasis.
Discussion: Esophageal and gastric cancer risks are modulated by multiple factors, including genetic susceptibility modifying environmental factors. Synchronous GEJ and gastric adenocarcinoma are rare and often confused with recurrence or metastasis of malignant tumors. Inactivation of the TP53 gene plays a crucial role in the formation of solid GI tumors
Disclosures:
Aireen Agulto, MD1, Harleen K. Chela, MD2, Ghassan Hammoud, MD, MPH3. D0715 - Synchronous Gastroesophageal Junction and Gastric Adenocarcinoma in an Otherwise Healthy Male, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Missouri Health Care, Columbia, MO; 2University of Missouri-Columbia, Columbia, MO; 3University of Missouri Health Care, Columbia, MO
Introduction: The incidence of multiple primary carcinomas (MPCs) is increasing but remains a rare diagnosis. MPCs are two or more unrelated cancers in one patient. The development of MPCs is theorized to be related to unhealthy lifestyles and genetic susceptibility. We present a previously healthy male without family history of GI malignancy diagnosed with synchronous gastroesophageal junction (GEJ) and gastric adenocarcinoma.
Case Description/Methods: A 41-year-old male without prior medical history presented with recent onset solid food dysphagia associated with worsening abdominal pain, weight loss, and dyspnea for 5 months. He denied alcohol or tobacco use, or family history of malignancy. Labs showed normal CEA and CA 19-9, and Computed Tomography (CT) of the chest and abdomen revealed bilateral pleural effusion with left lung collapse, numerous pulmonary nodules and enlarged mediastinal and abdominal lymph nodes (Figure A-B). There was a circumferential esophageal thickening at the GEJ and a concern for interstitial edematous pancreatitis (Figure C-D). Magnetic Resonance Imaging (MRI) of the abdomen revealed mesenteric nodularity concerning for peritoneal carcinomatosis and diffuse gastric wall and GEJ thickening concerning for malignancy (Figure E). His QuantiFERON-TB Gold (QFT) was positive, but AFB smears and PCR test were negative, consistent with latent TB. Upper GI endoscopy revealed extensive nodularity of the esophageal and gastric mucosa with a large ulcerated GEJ mass (Figure F-J). Gastric and esophageal biopsies revealed invasive adenocarcinoma with a differential expression of p53 staining, extensive mucinous features but without signet ring cells. Pleural and peritoneal fluid cytology were consistent with metastatic adenocarcinoma of primary GI origin. His hospital course was complicated by recurrent pleural effusions, pulmonary embolism and upper gastrointestinal bleeding. Patient was followed with oncology for chemoradiation therapy for advanced unresectable gastric and GEJ adenocarcinoma with distant metastasis.
Discussion: Esophageal and gastric cancer risks are modulated by multiple factors, including genetic susceptibility modifying environmental factors. Synchronous GEJ and gastric adenocarcinoma are rare and often confused with recurrence or metastasis of malignant tumors. Inactivation of the TP53 gene plays a crucial role in the formation of solid GI tumors
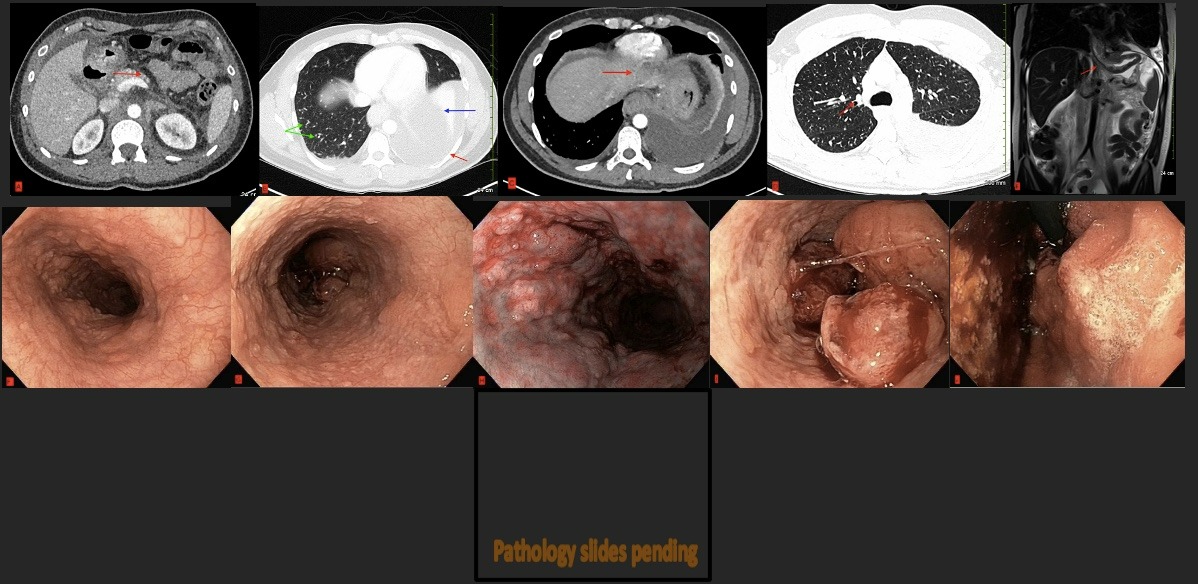
Figure: Figure A: CT A/P (axial) showing findings concerning for interstitial edematous pancreatitis (red arrow).
Figure B: CT A/P (axial) showing moderate left pleural effusion associated with multisegmental left lower lobe collapse (red and blue arrows) and numerous pulmonary nodules (green arrows).
Figure C: CT Chest (axial) showing diffuse circumferential esophageal and gastric wall thickening, most pronounced at the gastroesophageal junction (red arrow).
Figure D: CT Chest (axial) showing innumerable bilateral solid pulmonary nodules and mild mediastinal and upper abdominal lymphadenopathy (red arrow).
Figure E: MRIA/P (coronal) showing diffuse wall thickening of the gastroesophageal junction and stomach (red arrow).
Figure F: Endoscopy of distal esophagus demonstrating mucosaL nodularity.
Figure G: Endoscopy of proximal esophagus demonstrating nodularity.
Figure H: Endoscopy of esophagus under narrow band imaging, demonstrating nodularity and mucosal changes.
Figure I: Endoscopy showing large fungating GEJ mass with mucosal bleeding.
Figure J: Retroflexion view of large fungating GEJ mass with extensive gastric mucosal nodularity.
Pathology slides: Pathology slides of biopsies with p53 stain demonstrating differential p53 stain where poorly differentiated areas had a positive expression and loss of expression in better differentiated areas. Final genetics: pMMR, MSI-stable, TMB 3, no actionable mutations, HER2 FISH negative. MSH6 VUS was detected; genetics evaluation also showed MSH6 VUS; PDL1 IHC 1% (CPS).
Figure B: CT A/P (axial) showing moderate left pleural effusion associated with multisegmental left lower lobe collapse (red and blue arrows) and numerous pulmonary nodules (green arrows).
Figure C: CT Chest (axial) showing diffuse circumferential esophageal and gastric wall thickening, most pronounced at the gastroesophageal junction (red arrow).
Figure D: CT Chest (axial) showing innumerable bilateral solid pulmonary nodules and mild mediastinal and upper abdominal lymphadenopathy (red arrow).
Figure E: MRIA/P (coronal) showing diffuse wall thickening of the gastroesophageal junction and stomach (red arrow).
Figure F: Endoscopy of distal esophagus demonstrating mucosaL nodularity.
Figure G: Endoscopy of proximal esophagus demonstrating nodularity.
Figure H: Endoscopy of esophagus under narrow band imaging, demonstrating nodularity and mucosal changes.
Figure I: Endoscopy showing large fungating GEJ mass with mucosal bleeding.
Figure J: Retroflexion view of large fungating GEJ mass with extensive gastric mucosal nodularity.
Pathology slides: Pathology slides of biopsies with p53 stain demonstrating differential p53 stain where poorly differentiated areas had a positive expression and loss of expression in better differentiated areas. Final genetics: pMMR, MSI-stable, TMB 3, no actionable mutations, HER2 FISH negative. MSH6 VUS was detected; genetics evaluation also showed MSH6 VUS; PDL1 IHC 1% (CPS).
Disclosures:
Aireen Agulto indicated no relevant financial relationships.
Harleen Chela indicated no relevant financial relationships.
Ghassan Hammoud indicated no relevant financial relationships.
Aireen Agulto, MD1, Harleen K. Chela, MD2, Ghassan Hammoud, MD, MPH3. D0715 - Synchronous Gastroesophageal Junction and Gastric Adenocarcinoma in an Otherwise Healthy Male, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
