Back

Poster Session E - Tuesday Afternoon
Category: Colon
E0136 - Drug-Induced Colitis Secondary to Leflunomide
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Sherin Samuel, DO
UMass Chan Medical School - Baystate
Springfield, MA
Presenting Author(s)
Sherin Samuel, DO, Bushra Zia, MD, Jacob Alexander, MD
UMass Chan Medical School - Baystate, Springfield, MA
Introduction: Leflunomide is a disease modifying antirheumatic drug that works by inhibition of de novo pyrimidine synthesis resulting in antiproliferative and anti-inflammatory effects. Though diarrhea is the most common side effect of leflunomide, it is typically self-limited. Overt colitis induced by leflunomide is distinctly rare, with only a few cases in literature. We report a case of leflunomide-induced colitis that was initially misdiagnosed as ulcerative colitis.
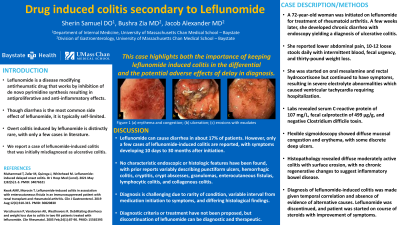
Case Description/Methods: A 72-year-old woman was initiated on leflunomide for treatment of rheumatoid arthritis. A few weeks later, she developed chronic diarrhea with endoscopy yielding a diagnosis of ulcerative colitis. She was started on oral mesalamine and rectal hydrocortisone but continued to have symptoms, resulting in severe electrolyte abnormalities which caused ventricular tachycardia requiring hospitalization. She reported lower abdominal pain, 10-12 loose stools daily with intermittent blood, fecal urgency, and thirty-pound weight loss. Labs revealed serum C-reactive protein of 107 mg/L, fecal calprotectin of 499 µg/g, and negative Clostridium difficile toxin. Flexible sigmoidoscopy showed diffuse mucosal congestion and erythema, with some discrete deep ulcers. Histopathology revealed diffuse moderately active colitis with surface erosion, with no chronic regenerative changes to suggest inflammatory bowel disease. Diagnosis of leflunomide-induced colitis was made given temporal correlation and absence of evidence of alternative causes. Leflunomide was discontinued, and patient was started on course of steroids with improvement of symptoms.
Discussion: Leflunomide can cause diarrhea in about 17% of patients. However, only a few cases of leflunomide-induced colitis are reported, with symptoms developing 10 days to 30 months after initiation. No characteristic endoscopic or histologic features have been found, with prior reports variably describing punctiform ulcers, hemorrhagic colitis, cryptitis, crypt abscesses, granulomas, enterocutaneous fistulas, lymphocytic colitis, and collagenous colitis. Diagnosis is challenging due to rarity of condition, variable interval from medication initiation to symptoms, and differing histological findings. Diagnostic criteria or treatment have not been proposed, but discontinuation of leflunomide can be diagnostic and therapeutic. This case highlights both the importance of keeping leflunomide-induced colitis in the differential and the potential adverse effects of delay in diagnosis.

Disclosures:
Sherin Samuel, DO, Bushra Zia, MD, Jacob Alexander, MD. E0136 - Drug-Induced Colitis Secondary to Leflunomide, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
UMass Chan Medical School - Baystate, Springfield, MA
Introduction: Leflunomide is a disease modifying antirheumatic drug that works by inhibition of de novo pyrimidine synthesis resulting in antiproliferative and anti-inflammatory effects. Though diarrhea is the most common side effect of leflunomide, it is typically self-limited. Overt colitis induced by leflunomide is distinctly rare, with only a few cases in literature. We report a case of leflunomide-induced colitis that was initially misdiagnosed as ulcerative colitis.
Case Description/Methods: A 72-year-old woman was initiated on leflunomide for treatment of rheumatoid arthritis. A few weeks later, she developed chronic diarrhea with endoscopy yielding a diagnosis of ulcerative colitis. She was started on oral mesalamine and rectal hydrocortisone but continued to have symptoms, resulting in severe electrolyte abnormalities which caused ventricular tachycardia requiring hospitalization. She reported lower abdominal pain, 10-12 loose stools daily with intermittent blood, fecal urgency, and thirty-pound weight loss. Labs revealed serum C-reactive protein of 107 mg/L, fecal calprotectin of 499 µg/g, and negative Clostridium difficile toxin. Flexible sigmoidoscopy showed diffuse mucosal congestion and erythema, with some discrete deep ulcers. Histopathology revealed diffuse moderately active colitis with surface erosion, with no chronic regenerative changes to suggest inflammatory bowel disease. Diagnosis of leflunomide-induced colitis was made given temporal correlation and absence of evidence of alternative causes. Leflunomide was discontinued, and patient was started on course of steroids with improvement of symptoms.
Discussion: Leflunomide can cause diarrhea in about 17% of patients. However, only a few cases of leflunomide-induced colitis are reported, with symptoms developing 10 days to 30 months after initiation. No characteristic endoscopic or histologic features have been found, with prior reports variably describing punctiform ulcers, hemorrhagic colitis, cryptitis, crypt abscesses, granulomas, enterocutaneous fistulas, lymphocytic colitis, and collagenous colitis. Diagnosis is challenging due to rarity of condition, variable interval from medication initiation to symptoms, and differing histological findings. Diagnostic criteria or treatment have not been proposed, but discontinuation of leflunomide can be diagnostic and therapeutic. This case highlights both the importance of keeping leflunomide-induced colitis in the differential and the potential adverse effects of delay in diagnosis.

Figure: Figure 1 (a) erythema and congestion, (b) ulceration, (c) erosions with exudates
Disclosures:
Sherin Samuel indicated no relevant financial relationships.
Bushra Zia indicated no relevant financial relationships.
Jacob Alexander indicated no relevant financial relationships.
Sherin Samuel, DO, Bushra Zia, MD, Jacob Alexander, MD. E0136 - Drug-Induced Colitis Secondary to Leflunomide, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
