Back

Poster Session B - Monday Morning
Category: Stomach
B0711 - Cellulase With Prokinetics Is an Effective Dissolution Therapy for Gastric Phytobezoars
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
Kwabena O. Adu-Gyamfi, MBChB
Medical College of Georgia - Augusta University
Augusta, GA
Presenting Author(s)
Award: Presidential Poster Award
Kwabena O. Adu-Gyamfi, MBChB1, Praneeth Kudaravalli, MD2, Satish Rao, MD3
1Medical College of Georgia - Augusta University, Augusta, GA; 2Augusta University Medical Center, Augusta, GA; 3Augusta University, Augusta, GA
Introduction: Gastric phytobezoars are hard concretions of ingested vegetable/food matter in the stomach. They can significantly impair mucosal visualization during esophagogastroduodenoscopy (EGD). In the absence of outlet obstruction, dissolution therapy is recommended as a first step whilst evaluating for underlying causes. Different dissolution therapies for bezoar have been described. Cellulase, although first described in 1980’s has not been systematically examined and whether combined therapy with prokinetics is more effective is unknown. We describe two patients with large gastric phytobezoars found on EGD and successfully treated with cellulase plus adjuvant azithromycin for 5 days.
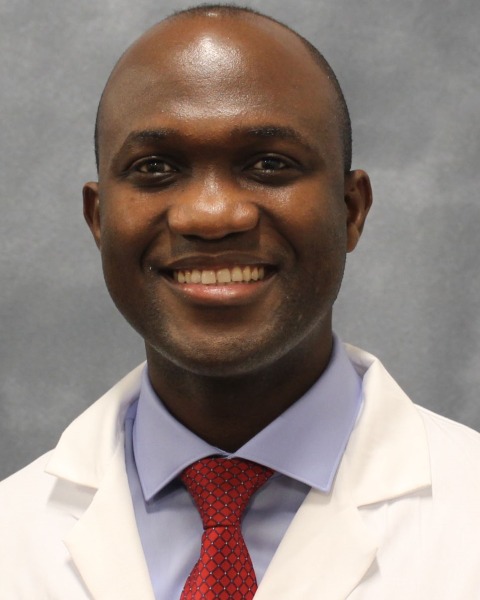
Case Description/Methods: Case 1: A 37-year-old Caucasian woman with type 2 diabetes mellitus (DM), gastroparesis and obesity presented with a 2-year history of worsening GERD, dyspepsia, early satiety and Gastroparesis Cardinal Symptom Index (GCSI) of 24. EGD revealed a large phytobezoar, occupying 60% of stomach (Fig 1a). She was treated with Cellulase 5g dissolved in 200ml of water, daily for 5 days on an empty stomach, and azithromycin 125mg liquid bid for 3 weeks. She reported significant symptom improvement in 1 week. Repeat EGD after 2-3 weeks showed normal stomach with no bezoar (Fig 1b), and GCSI improved to 18.
Case 2: A 64-year-old Caucasian woman with Type 2 DM and gastroparesis presented with worsening nausea, vomiting, early satiety and GCSI of 22. Examination noted mild epigastric fullness with tenderness and succussion splash. EGD noted a large gastric bezoar occupying the 75% of stomach. She was treated with aforementioned regimen. EGD after 2 weeks was normal with no bezoar (Fig 1c), and GCSI improved to 16.
Discussion: Gastric bezoars are rare with an estimated incidence of 0.3% on EGD. Risk factors include gastric dysmotility, gastric outlet obstruction, anticholinergic agents/opioids or psychiatric problems. They can be asymptomatic or cause abdominal pain, nausea, vomiting or early satiety. Agents used for chemical dissolution therapy (CDT) with varying results include cellulase, carbonated drinks, papain and acetylcysteine. Both of our patients had gastroparesis with poorly controlled DM and intolerance to metoclopramide. Possible risks of CDT include possible small bowel obstruction from partially dissolved bezoars. Combination therapy with Cellulase (5G), and Azithromycin (125 mg liquid bid, prokinetic) was safe and effective therapy for gastric phytobezoars without luminal obstruction.
Disclosures:
Kwabena O. Adu-Gyamfi, MBChB1, Praneeth Kudaravalli, MD2, Satish Rao, MD3. B0711 - Cellulase With Prokinetics Is an Effective Dissolution Therapy for Gastric Phytobezoars, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Kwabena O. Adu-Gyamfi, MBChB1, Praneeth Kudaravalli, MD2, Satish Rao, MD3
1Medical College of Georgia - Augusta University, Augusta, GA; 2Augusta University Medical Center, Augusta, GA; 3Augusta University, Augusta, GA
Introduction: Gastric phytobezoars are hard concretions of ingested vegetable/food matter in the stomach. They can significantly impair mucosal visualization during esophagogastroduodenoscopy (EGD). In the absence of outlet obstruction, dissolution therapy is recommended as a first step whilst evaluating for underlying causes. Different dissolution therapies for bezoar have been described. Cellulase, although first described in 1980’s has not been systematically examined and whether combined therapy with prokinetics is more effective is unknown. We describe two patients with large gastric phytobezoars found on EGD and successfully treated with cellulase plus adjuvant azithromycin for 5 days.
Case Description/Methods: Case 1: A 37-year-old Caucasian woman with type 2 diabetes mellitus (DM), gastroparesis and obesity presented with a 2-year history of worsening GERD, dyspepsia, early satiety and Gastroparesis Cardinal Symptom Index (GCSI) of 24. EGD revealed a large phytobezoar, occupying 60% of stomach (Fig 1a). She was treated with Cellulase 5g dissolved in 200ml of water, daily for 5 days on an empty stomach, and azithromycin 125mg liquid bid for 3 weeks. She reported significant symptom improvement in 1 week. Repeat EGD after 2-3 weeks showed normal stomach with no bezoar (Fig 1b), and GCSI improved to 18.
Case 2: A 64-year-old Caucasian woman with Type 2 DM and gastroparesis presented with worsening nausea, vomiting, early satiety and GCSI of 22. Examination noted mild epigastric fullness with tenderness and succussion splash. EGD noted a large gastric bezoar occupying the 75% of stomach. She was treated with aforementioned regimen. EGD after 2 weeks was normal with no bezoar (Fig 1c), and GCSI improved to 16.
Discussion: Gastric bezoars are rare with an estimated incidence of 0.3% on EGD. Risk factors include gastric dysmotility, gastric outlet obstruction, anticholinergic agents/opioids or psychiatric problems. They can be asymptomatic or cause abdominal pain, nausea, vomiting or early satiety. Agents used for chemical dissolution therapy (CDT) with varying results include cellulase, carbonated drinks, papain and acetylcysteine. Both of our patients had gastroparesis with poorly controlled DM and intolerance to metoclopramide. Possible risks of CDT include possible small bowel obstruction from partially dissolved bezoars. Combination therapy with Cellulase (5G), and Azithromycin (125 mg liquid bid, prokinetic) was safe and effective therapy for gastric phytobezoars without luminal obstruction.
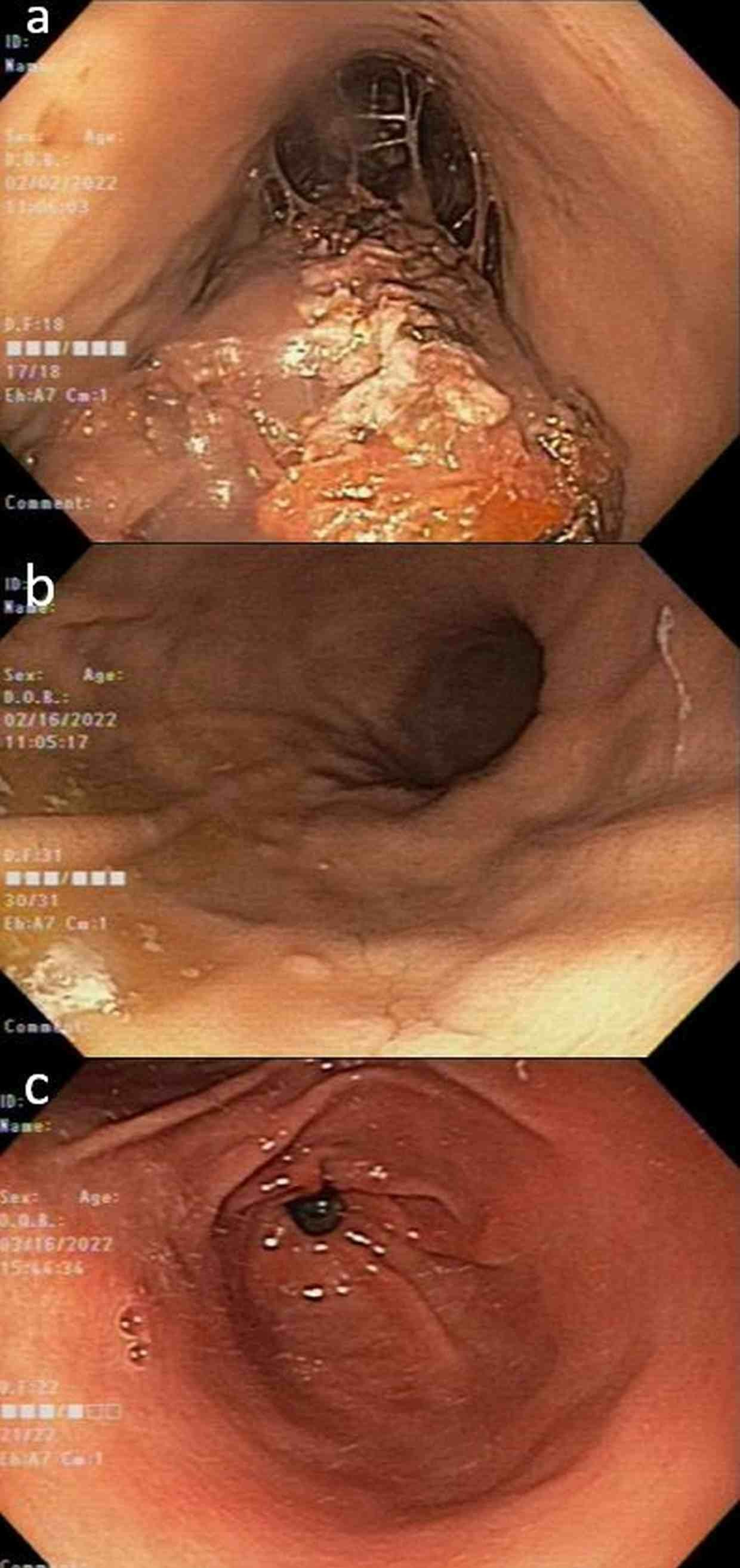
Figure: Fig 1. Endoscopic images (Patient 1) showing large phytobezoar (Fig 1a) and repeat EGD in 2 weeks showing normal stomach after dissolution therapy (Fig 1b). Normal EGD (patient 2) after dissolution therapy (Fig 1c).
Disclosures:
Kwabena Adu-Gyamfi indicated no relevant financial relationships.
Praneeth Kudaravalli indicated no relevant financial relationships.
Satish Rao: Salix Pharmaceuticals – Grant/Research Support. Vibrant – Advisor or Review Panel Member. Vibrant – Clinical Advisory Board.
Kwabena O. Adu-Gyamfi, MBChB1, Praneeth Kudaravalli, MD2, Satish Rao, MD3. B0711 - Cellulase With Prokinetics Is an Effective Dissolution Therapy for Gastric Phytobezoars, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

