Back

Poster Session A - Sunday Afternoon
Category: Pediatrics
A0603 - An Assessment of Pediatric ERCP Long-Term Quality of Life Outcomes
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio
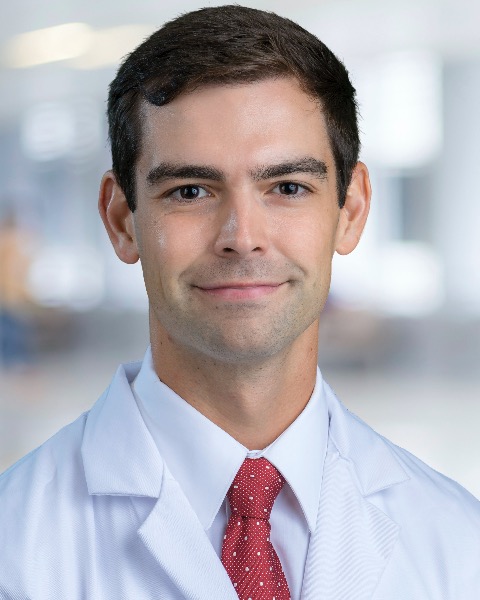
Eric Lorio, MD
Tulane University
Metairie, LA
Presenting Author(s)
Eric Lorio, MD1, Samuel N. Kahlenberg, MD2, Chris Moreau, BSBME3, Sandeep Patel, DO4
1Tulane University, Metairie, LA; 2University of North Carolina Hospitals, Chapel Hill, NC; 3UT Health San Antonio, San Antonio, TX; 4UT Health San Antonio, San Antonio, LA
Introduction: Due to its proven efficacy, endoscopic retrograde cholangiopancreatography (ERCP) is an increasingly used modality in pediatric populations, with utility extending to recurrent pancreatitis (the most common indication in children), chronic pancreatitis, and gallstone disease. However, little is known about long-term ERCP outcomes in pediatric patients. The goal of this project was to assess long-term quality-of-life outcomes in pediatric ERCP using a questionnaire previously validated for patients with chronic pancreatitis.
Methods: Adult patients who had an ERCP performed as a child at one of our three academic centers were contacted to assess their willingness to participate in the survey. A telephone script was utilized to reduce bias in the posing of questions. The questionnaire incorporated parts of pancreatitis quality of life instrument (PANQOLI), which has primarily been validated for chronic pancreatitis, as well as unique questions designed to evaluate distinctive problems posed by pancreatic and bile duct manipulation.
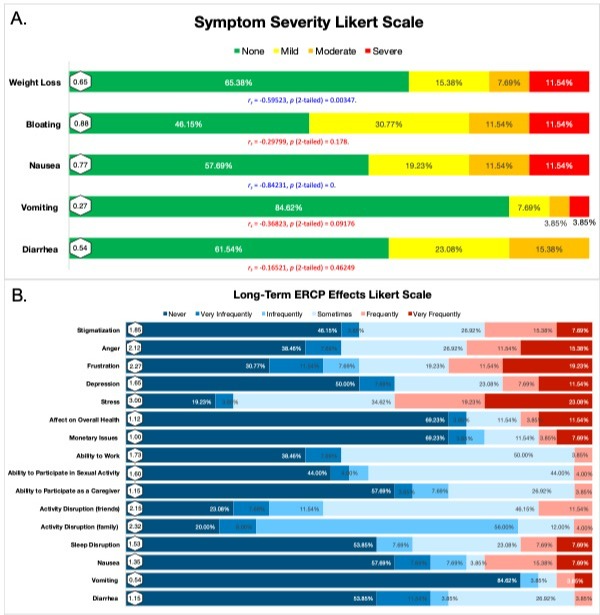
Results: 26 patients completed the questionnaire, with 46.15% reporting complete satisfaction with their health. Though only 23.08% recounted that their presenting symptoms were cured by ERCP (Table 1), the majority of patients (69.23%) perceived no effect of the prior ERCP on their overall health as adults. 34.61% of patients needed at least one additional ERCP, and a diagnosis of chronic pancreatitis was described by 42.31% of surveyed patients. Spearman correlation testing identified that increasing severity of nausea (rs = -0.84231) and weight loss (rs = -0.59523) correlated with decreases in patient health satisfaction (Figure 1A). 23.08% of patients continued to require pancreatic enzyme replacement into adulthood, and 4 of the 26 patients had prescriptions for opiate pain medication related to chronic abdominal pain. Very frequent stress and very frequent frustration were reported by 23.08% and 19.23% of patients, respectively (Figure 1B).
Discussion: This study offers a glimpse into the long-term physical, social, and emotional states of patients who underwent ERCP in childhood. Though we found that chronic symptoms related to ERCP contribute to decreased health satisfaction, further study is needed to assess risk factors for long-term complication in pediatric ERCP. A limitation of this study is the questionnaire’s reliance on patient recall, considering that many of these procedures were performed during childhood many years prior.
Disclosures:
Eric Lorio, MD1, Samuel N. Kahlenberg, MD2, Chris Moreau, BSBME3, Sandeep Patel, DO4. A0603 - An Assessment of Pediatric ERCP Long-Term Quality of Life Outcomes, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Tulane University, Metairie, LA; 2University of North Carolina Hospitals, Chapel Hill, NC; 3UT Health San Antonio, San Antonio, TX; 4UT Health San Antonio, San Antonio, LA
Introduction: Due to its proven efficacy, endoscopic retrograde cholangiopancreatography (ERCP) is an increasingly used modality in pediatric populations, with utility extending to recurrent pancreatitis (the most common indication in children), chronic pancreatitis, and gallstone disease. However, little is known about long-term ERCP outcomes in pediatric patients. The goal of this project was to assess long-term quality-of-life outcomes in pediatric ERCP using a questionnaire previously validated for patients with chronic pancreatitis.
Methods: Adult patients who had an ERCP performed as a child at one of our three academic centers were contacted to assess their willingness to participate in the survey. A telephone script was utilized to reduce bias in the posing of questions. The questionnaire incorporated parts of pancreatitis quality of life instrument (PANQOLI), which has primarily been validated for chronic pancreatitis, as well as unique questions designed to evaluate distinctive problems posed by pancreatic and bile duct manipulation.
Results: 26 patients completed the questionnaire, with 46.15% reporting complete satisfaction with their health. Though only 23.08% recounted that their presenting symptoms were cured by ERCP (Table 1), the majority of patients (69.23%) perceived no effect of the prior ERCP on their overall health as adults. 34.61% of patients needed at least one additional ERCP, and a diagnosis of chronic pancreatitis was described by 42.31% of surveyed patients. Spearman correlation testing identified that increasing severity of nausea (rs = -0.84231) and weight loss (rs = -0.59523) correlated with decreases in patient health satisfaction (Figure 1A). 23.08% of patients continued to require pancreatic enzyme replacement into adulthood, and 4 of the 26 patients had prescriptions for opiate pain medication related to chronic abdominal pain. Very frequent stress and very frequent frustration were reported by 23.08% and 19.23% of patients, respectively (Figure 1B).
Discussion: This study offers a glimpse into the long-term physical, social, and emotional states of patients who underwent ERCP in childhood. Though we found that chronic symptoms related to ERCP contribute to decreased health satisfaction, further study is needed to assess risk factors for long-term complication in pediatric ERCP. A limitation of this study is the questionnaire’s reliance on patient recall, considering that many of these procedures were performed during childhood many years prior.
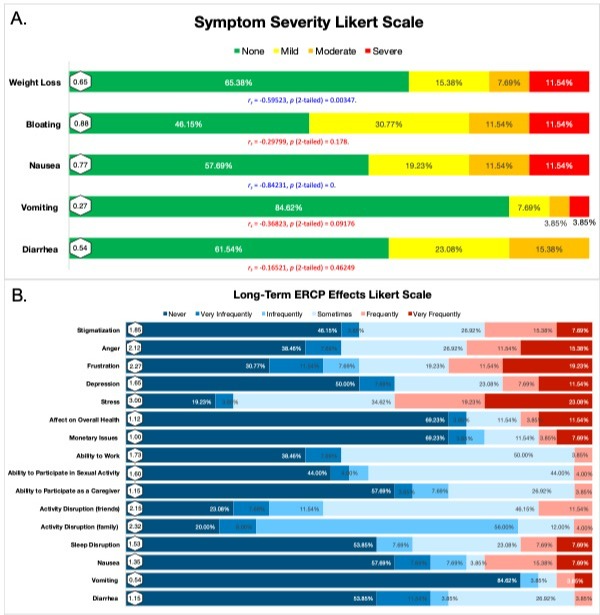
Figure: Figure 1: Likert tables showing response rates for reported symptom severity (A) and long-term effects from prior ERCP (B). Symptom severity scale (A) includes Spearman correlation coefficients which identified a correlation between increasing severity of nausea and weight loss and decreasing overall health satisfaction. A sizable number of patients reported stigmatization, anger, frustration, depression, or stress attributable to their prior disease course. There were also post-procedure limitations in the ability to work, participate in sexual activity, participate as a caregiver, and spend time with friends or family.
|
Table: Table 1: Of the 26 patients that completed our survey, only 23.08% reported that ERCP completely cured their presenting condition. 42.31% of patients reported chronic pancreatitis as a diagnosis after their ERCP, with 26.92% reporting an additional ERCP needed to address their presenting condition. The most common persistent symptoms were nausea, bloating, and weight loss.
Disclosures:
Eric Lorio indicated no relevant financial relationships.
Samuel Kahlenberg indicated no relevant financial relationships.
Chris Moreau indicated no relevant financial relationships.
Sandeep Patel indicated no relevant financial relationships.
Eric Lorio, MD1, Samuel N. Kahlenberg, MD2, Chris Moreau, BSBME3, Sandeep Patel, DO4. A0603 - An Assessment of Pediatric ERCP Long-Term Quality of Life Outcomes, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
