Back

Poster Session E - Tuesday Afternoon
Category: Biliary/Pancreas
E0081 - Pancreatitis Secondary to Paxlovid-Induced Tacrolimus Toxicity
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Michael Schwartz, MD
Cooper University Hospital
Camden, NJ
Presenting Author(s)
Michael Schwartz, MD1, Katherine Gheysens, MD1, Pilin Francis, DO1, Kunal K. Dalal, MD2
1Cooper University Hospital, Camden, NJ; 2Cooper University Hospital - Digestive Health Institute, Camden, NJ
Introduction: Pancreatitis is a very common gastrointestinal disease that results in hospital admission. Early detection and treatment leads to better outcomes. This is the first reported case of pancreatitis secondary to elevated tacrolimus in a patient with prior renal transplantation after receiving Paxlovid for a COVID-19 infection.
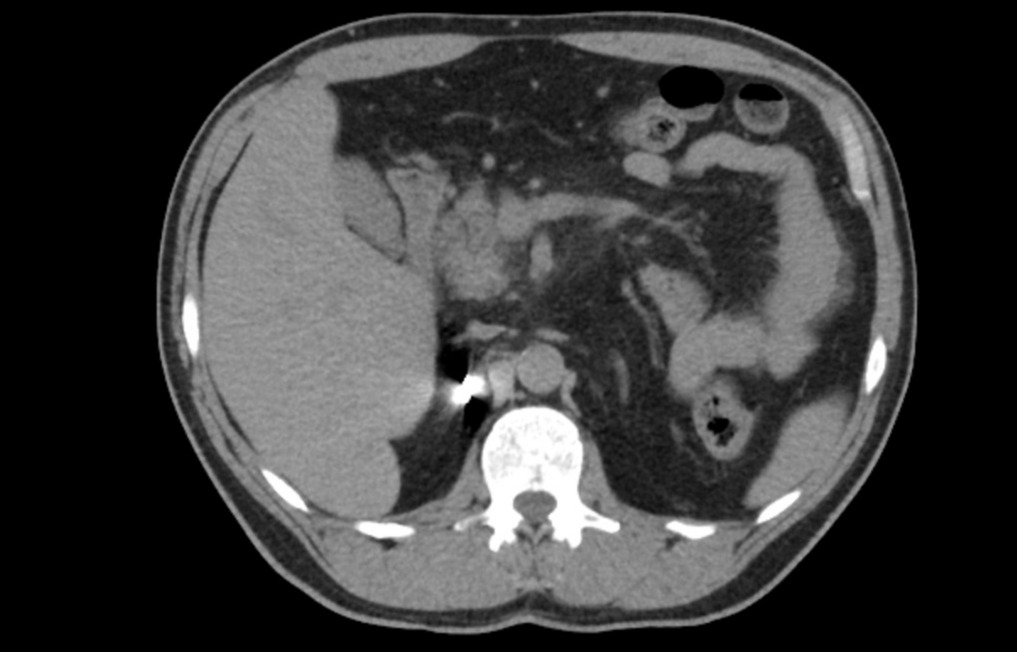
Case Description/Methods: A 57 year old male with past medical history of 4 renal transplants secondary to posterior urethral valves who presented to the emergency room with acute onset epigastric pain for 24 hours. He was on tacrolimus 5 mg every 48 hours monotherapy for his immunosuppression. 10 days prior to his presentation he had developed chills and anxiety. He tested positive for COVID-19 at that time on a home rapid test. His symptoms had not significantly improved and given his immunosuppressed state he was given Paxlovid (Nirmatrelvir/ritonavir). He took 2 days of Paxlovid, however after his second day of treatment he developed severe epigastric pain requiring him to go to the emergency room. On admission his labs were notable for a lipase of 150 U/L (ULN 63 U/L). He underwent a CT scan was notable for an enlarged pancreatic head and neck with peripancreatic fat stranding. He also had a right upper quadrant ultrasound without any cholelithiasis and only trace sludge noted. His creatinine was noted to be 1.81 mg/dl which was above his baseline of 1.2 mg/dl. His tacrolimus trough level resulted at a level 45.6 ng/ml and later peaked at 82.2 ng/ml. His liver enzymes were normal. He was treated as acute pancreatitis with hydration and his tacrolimus was held with overall clinical improvement.
Discussion: Tacrolimus is one of the most common medications used in solid organ transplantation. It is a calcineurin inhibitor that inhibits both T-lymphocyte signal transduction and IL-2 transcription. It is metabolized by the protein CYP3A and levels are monitored closely. Paxlovid is currently prescribed as an antiviral therapy for COVID-19 infection. The ritonavir compound in Paxlovid is potent inhibitor of CYP3A. Currently the guidelines do not recommend Paxlvoid as a therapeutic in patients taking tacrolimus as there is concern about increased drug levels. There have been several case reports of pancreatitis in setting of tacrolimus. This case report helps to demonstrate the need for close monitoring of therapeutics levels, especially in medications with high risk of drug to drug interaction to help prevent serious side effects such as tacrolimus induced pancreatitis.
Disclosures:
Michael Schwartz, MD1, Katherine Gheysens, MD1, Pilin Francis, DO1, Kunal K. Dalal, MD2. E0081 - Pancreatitis Secondary to Paxlovid-Induced Tacrolimus Toxicity, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Cooper University Hospital, Camden, NJ; 2Cooper University Hospital - Digestive Health Institute, Camden, NJ
Introduction: Pancreatitis is a very common gastrointestinal disease that results in hospital admission. Early detection and treatment leads to better outcomes. This is the first reported case of pancreatitis secondary to elevated tacrolimus in a patient with prior renal transplantation after receiving Paxlovid for a COVID-19 infection.
Case Description/Methods: A 57 year old male with past medical history of 4 renal transplants secondary to posterior urethral valves who presented to the emergency room with acute onset epigastric pain for 24 hours. He was on tacrolimus 5 mg every 48 hours monotherapy for his immunosuppression. 10 days prior to his presentation he had developed chills and anxiety. He tested positive for COVID-19 at that time on a home rapid test. His symptoms had not significantly improved and given his immunosuppressed state he was given Paxlovid (Nirmatrelvir/ritonavir). He took 2 days of Paxlovid, however after his second day of treatment he developed severe epigastric pain requiring him to go to the emergency room. On admission his labs were notable for a lipase of 150 U/L (ULN 63 U/L). He underwent a CT scan was notable for an enlarged pancreatic head and neck with peripancreatic fat stranding. He also had a right upper quadrant ultrasound without any cholelithiasis and only trace sludge noted. His creatinine was noted to be 1.81 mg/dl which was above his baseline of 1.2 mg/dl. His tacrolimus trough level resulted at a level 45.6 ng/ml and later peaked at 82.2 ng/ml. His liver enzymes were normal. He was treated as acute pancreatitis with hydration and his tacrolimus was held with overall clinical improvement.
Discussion: Tacrolimus is one of the most common medications used in solid organ transplantation. It is a calcineurin inhibitor that inhibits both T-lymphocyte signal transduction and IL-2 transcription. It is metabolized by the protein CYP3A and levels are monitored closely. Paxlovid is currently prescribed as an antiviral therapy for COVID-19 infection. The ritonavir compound in Paxlovid is potent inhibitor of CYP3A. Currently the guidelines do not recommend Paxlvoid as a therapeutic in patients taking tacrolimus as there is concern about increased drug levels. There have been several case reports of pancreatitis in setting of tacrolimus. This case report helps to demonstrate the need for close monitoring of therapeutics levels, especially in medications with high risk of drug to drug interaction to help prevent serious side effects such as tacrolimus induced pancreatitis.
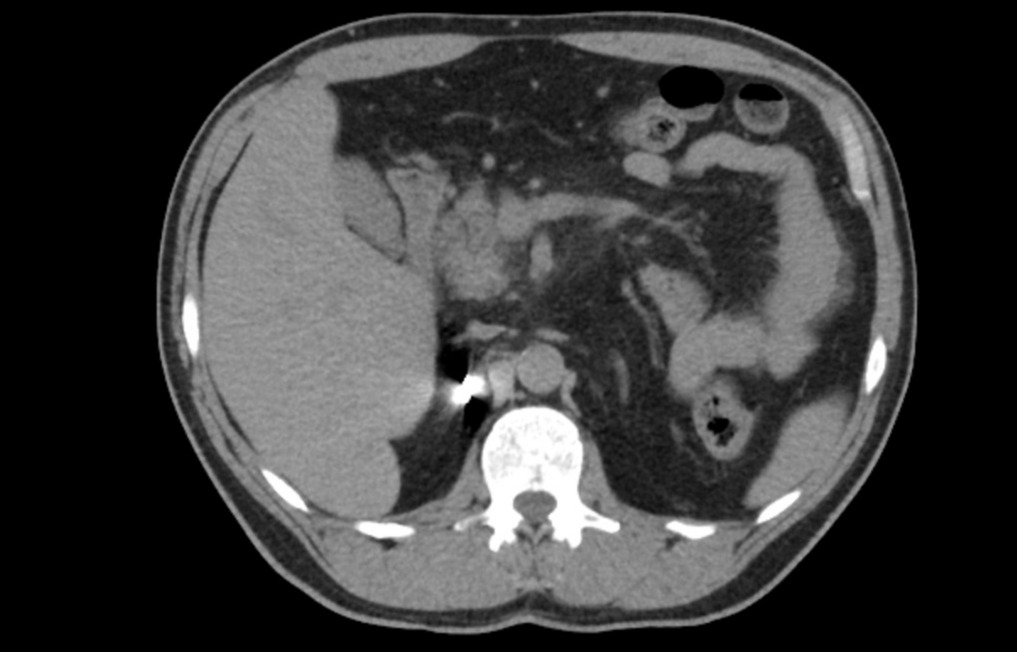
Figure: Axial image of acute pancreatitis. Noted enlarged pancreatic head and neck with peripancreatic fat stranding
Disclosures:
Michael Schwartz indicated no relevant financial relationships.
Katherine Gheysens indicated no relevant financial relationships.
Pilin Francis indicated no relevant financial relationships.
Kunal Dalal indicated no relevant financial relationships.
Michael Schwartz, MD1, Katherine Gheysens, MD1, Pilin Francis, DO1, Kunal K. Dalal, MD2. E0081 - Pancreatitis Secondary to Paxlovid-Induced Tacrolimus Toxicity, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
