Back

Poster Session B - Monday Morning
Category: Biliary/Pancreas
B0083 - Intrapancreatic Accessory Spleen, an Important Consideration That Can Reduce Invasive Interventions in the Evaluation of Pancreatic Lesions
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Muhammad Ali Butt, MD, MBBS
Allegheny General Hospital
Pittsburgh, PA
Presenting Author(s)
Muhammad Ali Butt, MD, MBBS1, Tabeer Rana, DO1, Tiana Dodd, DO2, Ramiro De La Guerra, MD1, Evan Reinhart, DO1, Suzanne Morrissey, MD1
1Allegheny General Hospital, Pittsburgh, PA; 2West Virginia School of Osteopathic Medicine, Lewisburg, WV
Introduction: The evaluation, diagnosis and management of pancreatic lesions is determined by radiographic imaging and Endoscopic Ultrasound with biopsy. We present a case of a pancreatic tail lesion that highlights the importance of considering an intrapancreatic accessory spleen within a differential diagnosis.
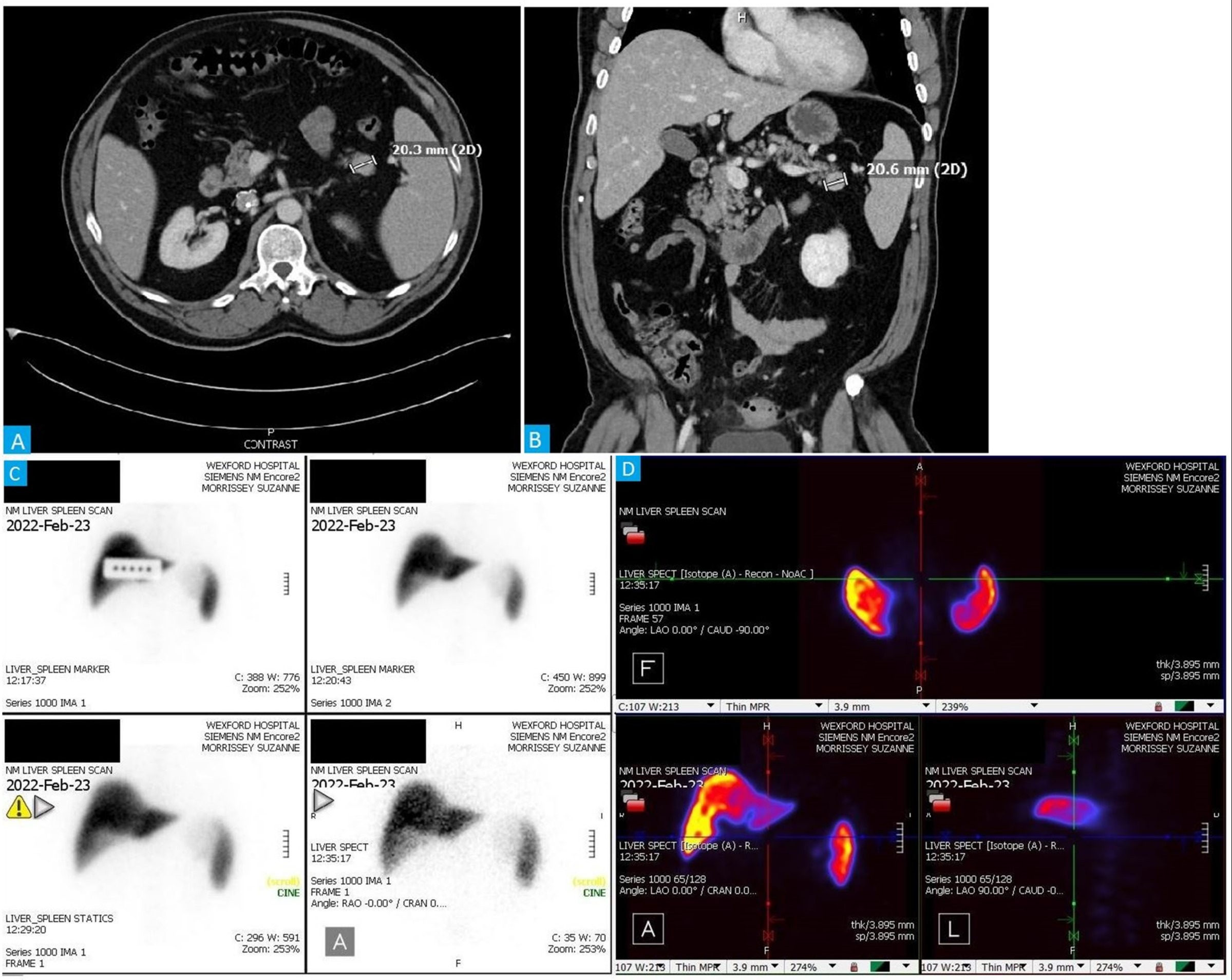
Case Description/Methods: A 48 year old Caucasian male with a past medical history significant for recurrent sigmoidal diverticulitis (complicated by a para-colonic abscess) and Clostridium difficile colitis who presented to an outpatient appointment for the evaluation of a pancreatic tail lesion that was incidentally identified on a CT abdomen/pelvis with contrast which was present on prior imaging dating back to three years time. On presentation, the patient endorsed that he was asymptomatic and specifically denied abdominal pain, nausea, vomiting, diarrhea, early satiety, weight loss, jaundice, flushing or hypoglycemia. The patient denied a personal or family history of pancreatitis or pancreatic cancer. Physical examination revealed that the patient was without scleral icterus, jaundice and had a benign abdominal exam. Lab findings revealed a normal complete blood count, complete metabolic panel and lipase level. CT abdomen/pelvis with contrast was reviewed which revealed a 2.1 cm hyperdense, hypervascular lesion localized within the pancreatic tail which was concerning for a pancreatic neuroendocrine tumor.
Upon detailed review, the patient was determined a suitable candidate for EUS with biopsy. However, the patient was concerned regarding the risk of malignant seeding with transgastric biopsy. Prior to proceeding with biopsy Gastroenterology recommended a Nuclear Medicine liver spleen scan to rule out the presence of an intrapancreatic accessory spleen, as its presence would eliminate the need for invasive interventions. A NM scan was performed which revealed a 2.1 cm contrast-enhancing soft tissue density in the pancreatic tail, which was most compatible with intrapancreatic accessory spleen. No further diagnostic or therapeutic interventions were required given the benign nature of the patient's diagnosis.
Discussion: This case highlights the importance of the consideration of an intrapancreatic accessory spleen during the evaluation of pancreatic body and tail lesions, as clinicians can prevent unnecessary invasive diagnostic and surgical procedures ultimately reducing patient morbidity and mortality.
Disclosures:
Muhammad Ali Butt, MD, MBBS1, Tabeer Rana, DO1, Tiana Dodd, DO2, Ramiro De La Guerra, MD1, Evan Reinhart, DO1, Suzanne Morrissey, MD1. B0083 - Intrapancreatic Accessory Spleen, an Important Consideration That Can Reduce Invasive Interventions in the Evaluation of Pancreatic Lesions, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Allegheny General Hospital, Pittsburgh, PA; 2West Virginia School of Osteopathic Medicine, Lewisburg, WV
Introduction: The evaluation, diagnosis and management of pancreatic lesions is determined by radiographic imaging and Endoscopic Ultrasound with biopsy. We present a case of a pancreatic tail lesion that highlights the importance of considering an intrapancreatic accessory spleen within a differential diagnosis.
Case Description/Methods: A 48 year old Caucasian male with a past medical history significant for recurrent sigmoidal diverticulitis (complicated by a para-colonic abscess) and Clostridium difficile colitis who presented to an outpatient appointment for the evaluation of a pancreatic tail lesion that was incidentally identified on a CT abdomen/pelvis with contrast which was present on prior imaging dating back to three years time. On presentation, the patient endorsed that he was asymptomatic and specifically denied abdominal pain, nausea, vomiting, diarrhea, early satiety, weight loss, jaundice, flushing or hypoglycemia. The patient denied a personal or family history of pancreatitis or pancreatic cancer. Physical examination revealed that the patient was without scleral icterus, jaundice and had a benign abdominal exam. Lab findings revealed a normal complete blood count, complete metabolic panel and lipase level. CT abdomen/pelvis with contrast was reviewed which revealed a 2.1 cm hyperdense, hypervascular lesion localized within the pancreatic tail which was concerning for a pancreatic neuroendocrine tumor.
Upon detailed review, the patient was determined a suitable candidate for EUS with biopsy. However, the patient was concerned regarding the risk of malignant seeding with transgastric biopsy. Prior to proceeding with biopsy Gastroenterology recommended a Nuclear Medicine liver spleen scan to rule out the presence of an intrapancreatic accessory spleen, as its presence would eliminate the need for invasive interventions. A NM scan was performed which revealed a 2.1 cm contrast-enhancing soft tissue density in the pancreatic tail, which was most compatible with intrapancreatic accessory spleen. No further diagnostic or therapeutic interventions were required given the benign nature of the patient's diagnosis.
Discussion: This case highlights the importance of the consideration of an intrapancreatic accessory spleen during the evaluation of pancreatic body and tail lesions, as clinicians can prevent unnecessary invasive diagnostic and surgical procedures ultimately reducing patient morbidity and mortality.
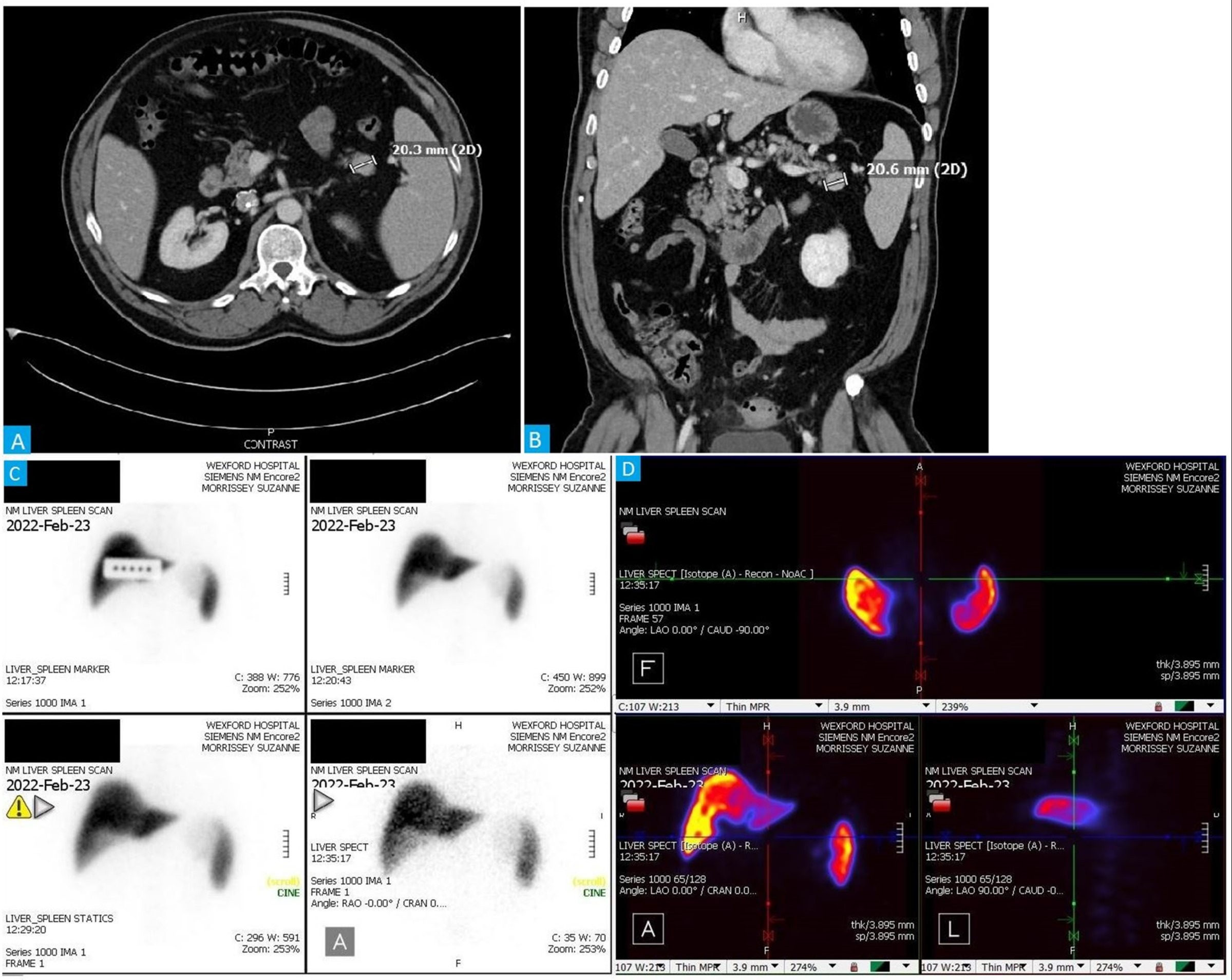
Figure: CT scan remarkable for Pancreatic tail lesion and NM scan showing 2.1 cm contrast-enhancing soft tissue density in the pancreatic tail, compatible with intrapancreatic accessory spleen.
Disclosures:
Muhammad Ali Butt indicated no relevant financial relationships.
Tabeer Rana indicated no relevant financial relationships.
Tiana Dodd indicated no relevant financial relationships.
Ramiro De La Guerra indicated no relevant financial relationships.
Evan Reinhart indicated no relevant financial relationships.
Suzanne Morrissey indicated no relevant financial relationships.
Muhammad Ali Butt, MD, MBBS1, Tabeer Rana, DO1, Tiana Dodd, DO2, Ramiro De La Guerra, MD1, Evan Reinhart, DO1, Suzanne Morrissey, MD1. B0083 - Intrapancreatic Accessory Spleen, an Important Consideration That Can Reduce Invasive Interventions in the Evaluation of Pancreatic Lesions, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
