Back

Poster Session B - Monday Morning
Category: Esophagus
B0247 - Candida-Necrotizing Esophagitis as a Cause of Upper GI Bleed in a Patient With Poorly Controlled Insulin-Dependent Diabetes Mellitus
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Malik Mushannen
Weill Cornell Medicine
New York, New York
Presenting Author(s)
Malik Mushannen, 1, Hasan Alroobi, 1, Suzanne Elshafey, MD2, Carl Crawford, MD3, David Wan, MD4
1Weill Cornell Medicine, New York, NY; 2New York Presbyterian-Weill Cornell Medical Center, Manhattan, NY; 3New York-Presbyterian Hospital/Weill Cornell Medical College, New York, NY; 4New York-Presbyterian Hospital/Weill Cornell Medicine, New York, NY
Introduction: Necrotizing esophagitis, also known as Black Esophagus, is a rare cause of upper gastrointestinal bleeding (GI). Patients can present with hematochezia or melena. The diagnosis is made on endoscopic evaluation with good prognosis if caught early.
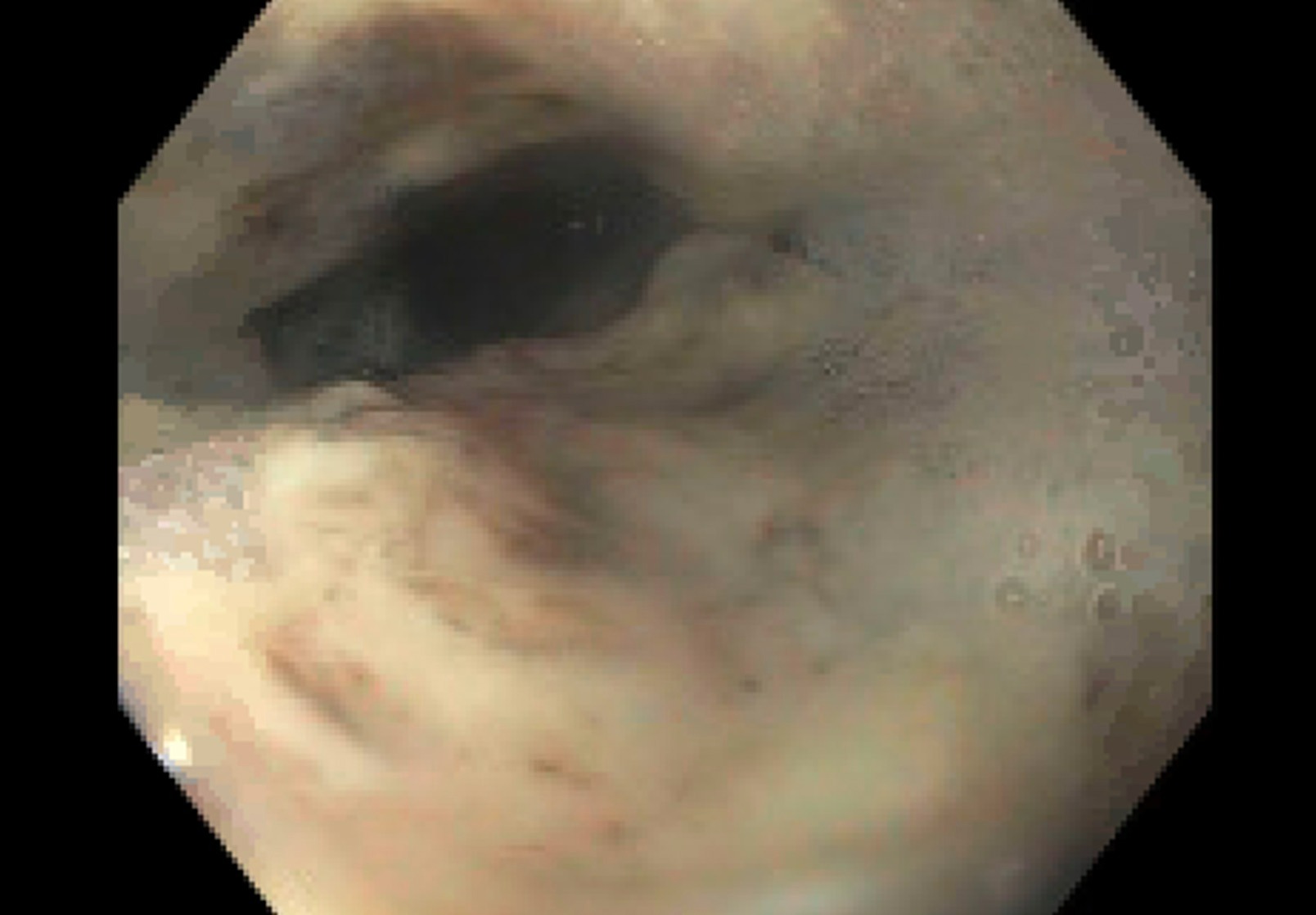
Case Description/Methods: A 27 year-old-woman with poorly controlled insulin dependent type I diabetes mellitus (hemoglobin A1c 15) requiring multiple admissions for diabetic ketoacidosis (DKA) presented to the emergency department with nausea and vomiting. She was found to have a hemoglobin of 9.2 g/dL down from 11.2 g.dL. CT scan showed diffuse esophageal wall thickening. She left the emergency department AMA without further treatment but re-presented four days later with persistent symptoms. She reported chronic, repeated self-induced emesis to alleviate symptoms of early satiety. Initial emesis was bilious but subsequently changed to dark red after repeat bouts of emesis. Repeat labs showed significant metabolic acidosis with pH 7.04, anion gap >20, hyperglycemia >600, and hemoglobin now of 4.5 g/dL. She was admitted to the medical intensive care unit for management of DKA and bloody emesis. She received four units packed red blood cells with appropriate hemoglobin response to 8.0 g/dL. The gastroenterology service was consulted and performed an esophagogastroduodenoscopy. It revealed severe, diffuse ulceration throughout the entire esophagus with stigmata of recent bleeding (Figure 1). Biopsies showed numerous fungal forms consistent with candidiasis as well as features of necrotizing esophagitis. A diagnosis of candida and necrotizing esophagitis was made. She was started on fluconazole daily and twice daily proton pump inhibitor. Unfortunately, she was seen in clinic once and then lost to follow up.
Discussion: Necrotizing esophagitis is a rare cause of acute GI bleed with unknown etiology. This disease is associated with DKA (likely due to volume depletion), hypoxia, carcinoma and ischemic events. Management includes fluid and blood product resuscitation, and treatment of the underlying disease. Complications include the development of esophageal strictures or perforation. Overall mortality is low, with the underlying disease being the cause of death in most instances. In this patient, endoscopic evaluation was key to establish the cause of her bleeding. Treatment of her candida and strict glycemic control were key for medical optimization that led to successful discharge and no re-bleeding episodes for the 3 weeks she remained for follow up.
Disclosures:
Malik Mushannen, 1, Hasan Alroobi, 1, Suzanne Elshafey, MD2, Carl Crawford, MD3, David Wan, MD4. B0247 - Candida-Necrotizing Esophagitis as a Cause of Upper GI Bleed in a Patient With Poorly Controlled Insulin-Dependent Diabetes Mellitus, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Weill Cornell Medicine, New York, NY; 2New York Presbyterian-Weill Cornell Medical Center, Manhattan, NY; 3New York-Presbyterian Hospital/Weill Cornell Medical College, New York, NY; 4New York-Presbyterian Hospital/Weill Cornell Medicine, New York, NY
Introduction: Necrotizing esophagitis, also known as Black Esophagus, is a rare cause of upper gastrointestinal bleeding (GI). Patients can present with hematochezia or melena. The diagnosis is made on endoscopic evaluation with good prognosis if caught early.
Case Description/Methods: A 27 year-old-woman with poorly controlled insulin dependent type I diabetes mellitus (hemoglobin A1c 15) requiring multiple admissions for diabetic ketoacidosis (DKA) presented to the emergency department with nausea and vomiting. She was found to have a hemoglobin of 9.2 g/dL down from 11.2 g.dL. CT scan showed diffuse esophageal wall thickening. She left the emergency department AMA without further treatment but re-presented four days later with persistent symptoms. She reported chronic, repeated self-induced emesis to alleviate symptoms of early satiety. Initial emesis was bilious but subsequently changed to dark red after repeat bouts of emesis. Repeat labs showed significant metabolic acidosis with pH 7.04, anion gap >20, hyperglycemia >600, and hemoglobin now of 4.5 g/dL. She was admitted to the medical intensive care unit for management of DKA and bloody emesis. She received four units packed red blood cells with appropriate hemoglobin response to 8.0 g/dL. The gastroenterology service was consulted and performed an esophagogastroduodenoscopy. It revealed severe, diffuse ulceration throughout the entire esophagus with stigmata of recent bleeding (Figure 1). Biopsies showed numerous fungal forms consistent with candidiasis as well as features of necrotizing esophagitis. A diagnosis of candida and necrotizing esophagitis was made. She was started on fluconazole daily and twice daily proton pump inhibitor. Unfortunately, she was seen in clinic once and then lost to follow up.
Discussion: Necrotizing esophagitis is a rare cause of acute GI bleed with unknown etiology. This disease is associated with DKA (likely due to volume depletion), hypoxia, carcinoma and ischemic events. Management includes fluid and blood product resuscitation, and treatment of the underlying disease. Complications include the development of esophageal strictures or perforation. Overall mortality is low, with the underlying disease being the cause of death in most instances. In this patient, endoscopic evaluation was key to establish the cause of her bleeding. Treatment of her candida and strict glycemic control were key for medical optimization that led to successful discharge and no re-bleeding episodes for the 3 weeks she remained for follow up.
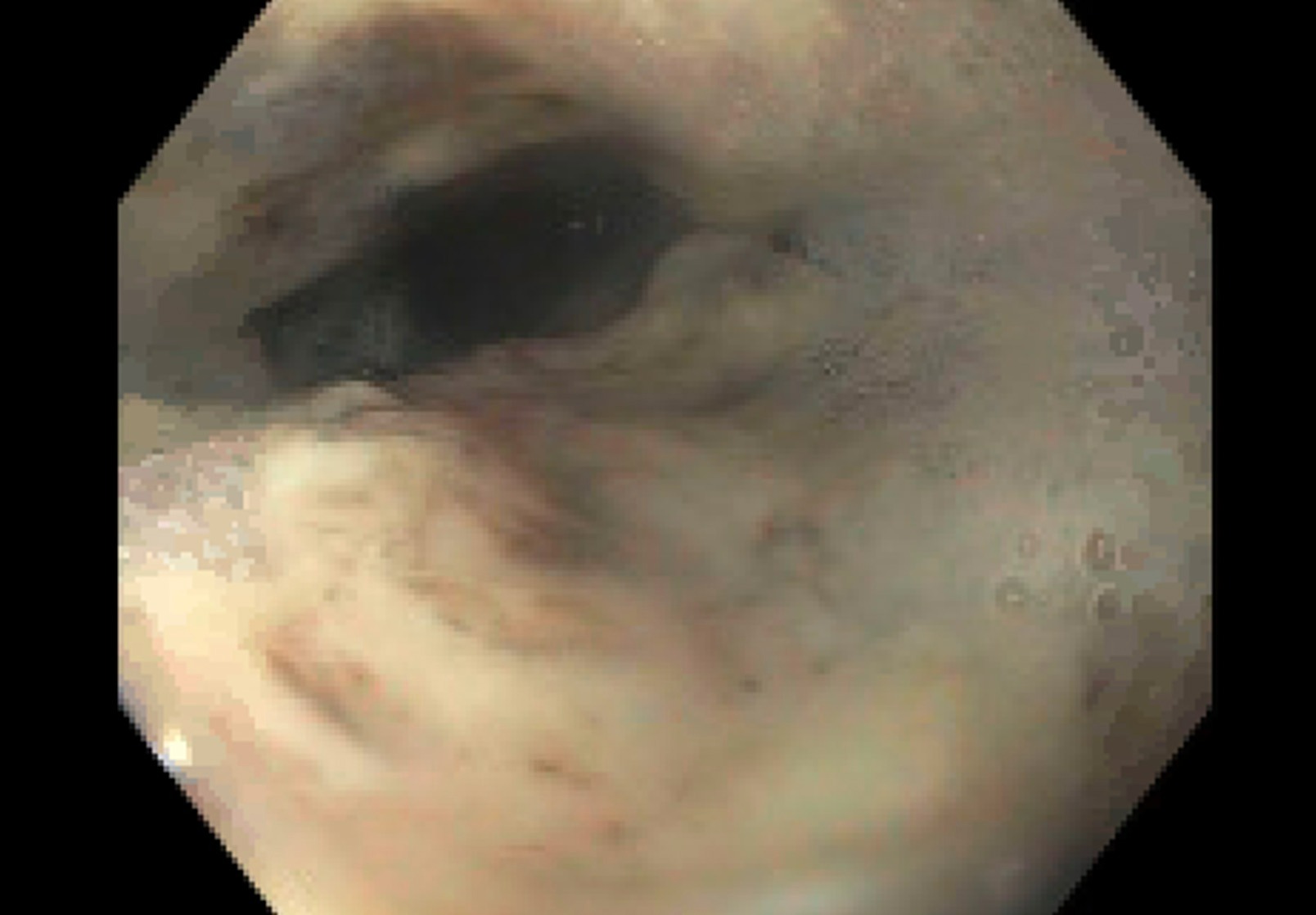
Figure: Endoscopic view of the lower esophagus revealing diffuse ulceration
Disclosures:
Malik Mushannen indicated no relevant financial relationships.
Hasan Alroobi indicated no relevant financial relationships.
Suzanne Elshafey indicated no relevant financial relationships.
Carl Crawford indicated no relevant financial relationships.
David Wan indicated no relevant financial relationships.
Malik Mushannen, 1, Hasan Alroobi, 1, Suzanne Elshafey, MD2, Carl Crawford, MD3, David Wan, MD4. B0247 - Candida-Necrotizing Esophagitis as a Cause of Upper GI Bleed in a Patient With Poorly Controlled Insulin-Dependent Diabetes Mellitus, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
