Back

Poster Session C - Monday Afternoon
Category: Stomach
C0733 - Adenocarcinoma of the Gastric Stump After Billroth II
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio
- NG
Nathan Grigg, DO
Parkview Medical Center
Pueblo, CO
Presenting Author(s)
Nathan Grigg, DO, Bryant Javier, DO, Rajiv Singh, MD, Daniel Heck, DO, Renuka Singh, MD, Christopher Calcagno, DO, Zachary Brodie, MS
Parkview Medical Center, Pueblo, CO
Introduction: Patients with a prior partial gastrectomy for benign diseases, such as Peptic Ulcer Disease (PUD), are at an increased risk of developing Gastric remnant Carcinomas which generally arise near the anastomotic site. Advancing therapeutics have reduced the prevalence of peptic ulcer gastrectomy, though it may still be indicated in certain instances including; bleeding, perforation, malignancy, and gastric outlet obstruction. Despite decreased gastrectomies performed, the long interval between surgery and the development of cancer has caused the incidence to remain stagnant.
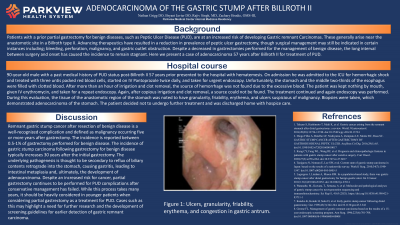
Case Description/Methods: A 90-year-old male with a history of PUD status post-Billroth II 57 years prior presented to the hospital with hematemesis. He was admitted to the ICU for hemorrhagic shock and treated with packed red blood cells, IV Pantoprazole, and taken for endoscopy. Unfortunately, the stomach and the middle two-thirds of the esophagus were filled with clotted blood. After more than an hour of irrigation and clot removal, the source of hemorrhage was not found due to the excessive blood. The patient was kept nothing by mouth, given IV erythromycin, and taken for a repeat endoscopy. Again, after copious irrigation and clot removal, a source could not be found. The treatment continued and again endoscopy was performed. During this evaluation, the tissue of the anastomotic region of the stomach was noted to have granularity, friability, erythema, and ulcers. Biopsies were taken, which demonstrated adenocarcinoma of the stomach. The patient decided not to undergo further treatment and was discharged home with hospice care.
Discussion: Remnant gastric stump cancer after resection of benign disease is a well-recognized complication and is defined as malignancy occurring five or more years after gastrectomy. The incidence is between 0.5-1% and typically increases 30 years after the initial gastrectomy. The underlying pathogenesis is thought to be secondary to reflux of biliary contents retrograde into the stomach, causing gastritis, leading to intestinal metaplasia, and the development of adenocarcinoma. Despite the risk, partial gastrectomy continues to be performed for PUD complications after conservative management has failed. While this process takes many years, it should be strongly considered in younger patients when considering partial gastrectomy. Cases such as this may highlight a need for further research and the development of screening guidelines for earlier detection of gastric remnant carcinoma.

Disclosures:
Nathan Grigg, DO, Bryant Javier, DO, Rajiv Singh, MD, Daniel Heck, DO, Renuka Singh, MD, Christopher Calcagno, DO, Zachary Brodie, MS. C0733 - Adenocarcinoma of the Gastric Stump After Billroth II, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Parkview Medical Center, Pueblo, CO
Introduction: Patients with a prior partial gastrectomy for benign diseases, such as Peptic Ulcer Disease (PUD), are at an increased risk of developing Gastric remnant Carcinomas which generally arise near the anastomotic site. Advancing therapeutics have reduced the prevalence of peptic ulcer gastrectomy, though it may still be indicated in certain instances including; bleeding, perforation, malignancy, and gastric outlet obstruction. Despite decreased gastrectomies performed, the long interval between surgery and the development of cancer has caused the incidence to remain stagnant.
Case Description/Methods: A 90-year-old male with a history of PUD status post-Billroth II 57 years prior presented to the hospital with hematemesis. He was admitted to the ICU for hemorrhagic shock and treated with packed red blood cells, IV Pantoprazole, and taken for endoscopy. Unfortunately, the stomach and the middle two-thirds of the esophagus were filled with clotted blood. After more than an hour of irrigation and clot removal, the source of hemorrhage was not found due to the excessive blood. The patient was kept nothing by mouth, given IV erythromycin, and taken for a repeat endoscopy. Again, after copious irrigation and clot removal, a source could not be found. The treatment continued and again endoscopy was performed. During this evaluation, the tissue of the anastomotic region of the stomach was noted to have granularity, friability, erythema, and ulcers. Biopsies were taken, which demonstrated adenocarcinoma of the stomach. The patient decided not to undergo further treatment and was discharged home with hospice care.
Discussion: Remnant gastric stump cancer after resection of benign disease is a well-recognized complication and is defined as malignancy occurring five or more years after gastrectomy. The incidence is between 0.5-1% and typically increases 30 years after the initial gastrectomy. The underlying pathogenesis is thought to be secondary to reflux of biliary contents retrograde into the stomach, causing gastritis, leading to intestinal metaplasia, and the development of adenocarcinoma. Despite the risk, partial gastrectomy continues to be performed for PUD complications after conservative management has failed. While this process takes many years, it should be strongly considered in younger patients when considering partial gastrectomy. Cases such as this may highlight a need for further research and the development of screening guidelines for earlier detection of gastric remnant carcinoma.

Figure: Ulcers, granularity, friability, erythema, and congestion in the gastric antrum.
Disclosures:
Nathan Grigg indicated no relevant financial relationships.
Bryant Javier indicated no relevant financial relationships.
Rajiv Singh indicated no relevant financial relationships.
Daniel Heck indicated no relevant financial relationships.
Renuka Singh indicated no relevant financial relationships.
Christopher Calcagno indicated no relevant financial relationships.
Zachary Brodie indicated no relevant financial relationships.
Nathan Grigg, DO, Bryant Javier, DO, Rajiv Singh, MD, Daniel Heck, DO, Renuka Singh, MD, Christopher Calcagno, DO, Zachary Brodie, MS. C0733 - Adenocarcinoma of the Gastric Stump After Billroth II, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
