Back

Poster Session B - Monday Morning
Category: Stomach
B0716 - Abdominal Wall Necrotizing Fasciitis in a Recent COVID-19 Infection as a Rare Complication of Percutaneous Endoscopic Gastrostomy: Case Report and Review of Literature
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Vishal Chandel, MD
Suburban Community Hospital
Norristown, PA
Presenting Author(s)
Vishal Chandel, MD1, Sridhar Reddy Patlolla, MD1, Imran Khokhar, MD1, Mathew Mathew, MD1, Robin Zachariah, MD2, Emad Mansoor, MD3
1Suburban Community Hospital, Norristown, PA; 2Duke Health, Durham, NC; 3University Hospital Medical Center, Cleveland, OH
Introduction: Complications of percutaneous endoscopic gastrostomy (PEG-tube) can be minor (wound infection, bleeding, ulceration, tube dysfunction, inadvertent removal, gastric outlet obstruction) or major (colo-cutaneous fistula, necrotizing fasciitis). Abdominal wall necrotizing fasciitis from a leaking or dislodged PEG-tube is a rare but life-threatening complication.
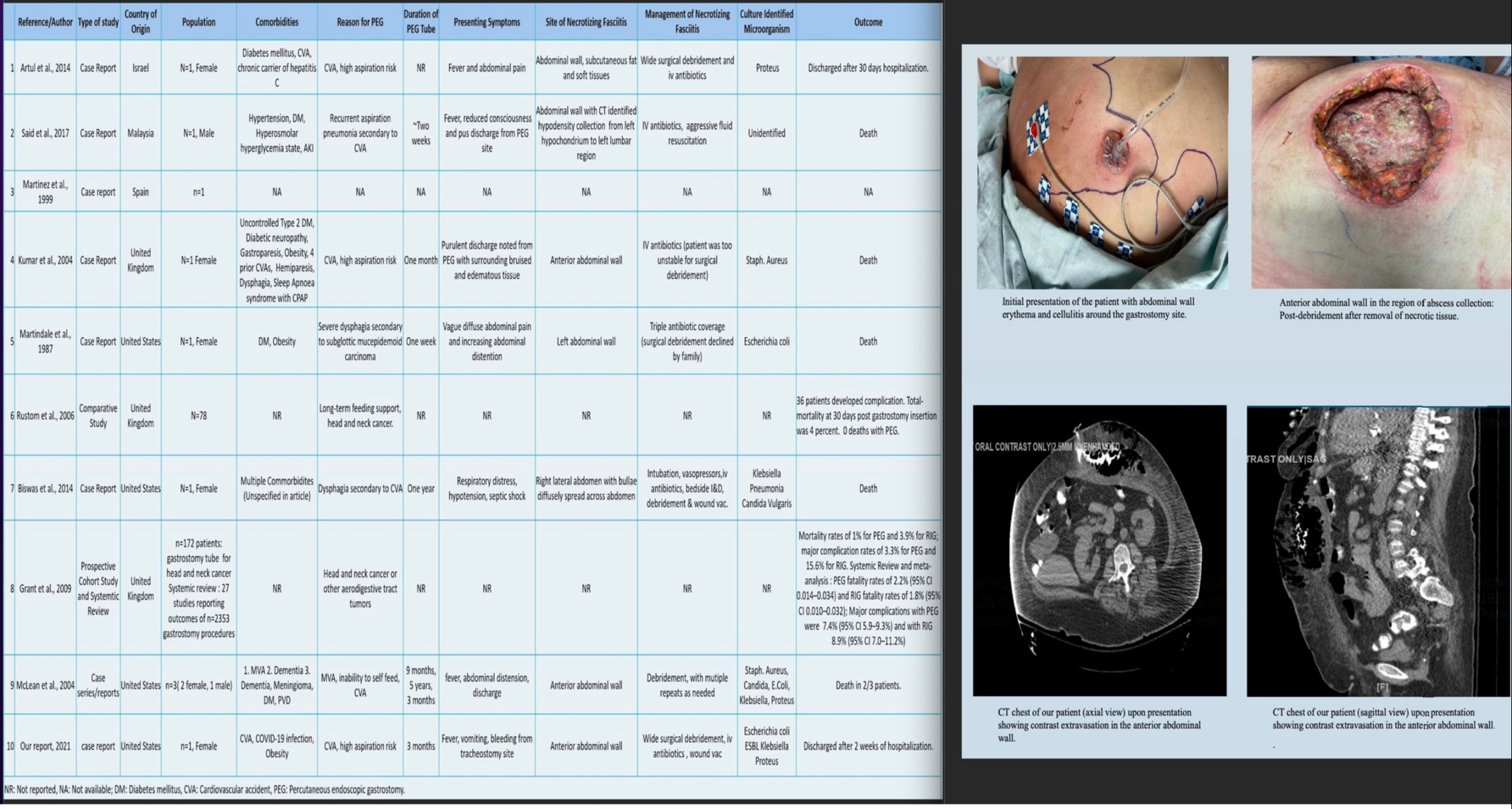
Case Description/Methods: A 65-year-old female with history of hypoxic respiratory failure, stroke (requiring tracheostomy and PEG-tube), recent COVID-infection, atrial fibrillation presented with fever, tachycardia, tachypnea, and leukocytosis. Examination showed decreased basal breath sounds, mild erythema around gastrostomy site, while abdomen had no peritoneal signs. CT-scan showed bilateral lower lobe consolidations and extensive subcutaneous emphysema throughout anterior abdominal wall tracking into subcutaneous soft tissues and fat stranding. Her abdominal erythema worsened on day-2 as rapidly progressing cellulitis, with diffuse tenderness and crepitus. Contrast radiography confirmed necrotizing fasciitis of the abdominal wall. Broad-spectrums antibiotics were initiated. Patient underwent surgical debridement, with removal of (15x20x20)cm necrotic tissue from anterior abdominal wall extending to fascial layers. Her wound cultures grew ESBL E.Coli, ESBL Klebsiella pneumonia and Enterococcus faecalis. Patient was discharged once stable; on wound-vac, dobhoff-tube nutrition and extended antibiotic regimen.
Discussion: Abdominal wall NF is a rare complication of PEG-tubes seen in less than 1% of gastrostomy procedures with mortality between 50-80%. Old age, obesity, diabetes mellitus, immunocompromised status, and even COVID-19 infection are risk factors. In our patient, leakage from the dislodged tube into abdominal wall caused infection by gas-producing organisms. Her recent COVID-19 infection and multiple medical comorbidities also clouded the initial presentation. Our review of literature included 5 case reports- 4 reported death as the final outcome, one comparative study demonstrated PEG tubes have greater safety and fewer complications compared to other gastrostomy techniques, and one systemic review reported major complication rate of 7.4% and fatality rate of 2.2% following PEG-placement. Since PEG-tubes are widely used in critically-ill patients, physicians must be aware of this rare but life-threatening complication and their silent manifestation in this COVID era.
Disclosures:
Vishal Chandel, MD1, Sridhar Reddy Patlolla, MD1, Imran Khokhar, MD1, Mathew Mathew, MD1, Robin Zachariah, MD2, Emad Mansoor, MD3. B0716 - Abdominal Wall Necrotizing Fasciitis in a Recent COVID-19 Infection as a Rare Complication of Percutaneous Endoscopic Gastrostomy: Case Report and Review of Literature, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Suburban Community Hospital, Norristown, PA; 2Duke Health, Durham, NC; 3University Hospital Medical Center, Cleveland, OH
Introduction: Complications of percutaneous endoscopic gastrostomy (PEG-tube) can be minor (wound infection, bleeding, ulceration, tube dysfunction, inadvertent removal, gastric outlet obstruction) or major (colo-cutaneous fistula, necrotizing fasciitis). Abdominal wall necrotizing fasciitis from a leaking or dislodged PEG-tube is a rare but life-threatening complication.
Case Description/Methods: A 65-year-old female with history of hypoxic respiratory failure, stroke (requiring tracheostomy and PEG-tube), recent COVID-infection, atrial fibrillation presented with fever, tachycardia, tachypnea, and leukocytosis. Examination showed decreased basal breath sounds, mild erythema around gastrostomy site, while abdomen had no peritoneal signs. CT-scan showed bilateral lower lobe consolidations and extensive subcutaneous emphysema throughout anterior abdominal wall tracking into subcutaneous soft tissues and fat stranding. Her abdominal erythema worsened on day-2 as rapidly progressing cellulitis, with diffuse tenderness and crepitus. Contrast radiography confirmed necrotizing fasciitis of the abdominal wall. Broad-spectrums antibiotics were initiated. Patient underwent surgical debridement, with removal of (15x20x20)cm necrotic tissue from anterior abdominal wall extending to fascial layers. Her wound cultures grew ESBL E.Coli, ESBL Klebsiella pneumonia and Enterococcus faecalis. Patient was discharged once stable; on wound-vac, dobhoff-tube nutrition and extended antibiotic regimen.
Discussion: Abdominal wall NF is a rare complication of PEG-tubes seen in less than 1% of gastrostomy procedures with mortality between 50-80%. Old age, obesity, diabetes mellitus, immunocompromised status, and even COVID-19 infection are risk factors. In our patient, leakage from the dislodged tube into abdominal wall caused infection by gas-producing organisms. Her recent COVID-19 infection and multiple medical comorbidities also clouded the initial presentation. Our review of literature included 5 case reports- 4 reported death as the final outcome, one comparative study demonstrated PEG tubes have greater safety and fewer complications compared to other gastrostomy techniques, and one systemic review reported major complication rate of 7.4% and fatality rate of 2.2% following PEG-placement. Since PEG-tubes are widely used in critically-ill patients, physicians must be aware of this rare but life-threatening complication and their silent manifestation in this COVID era.
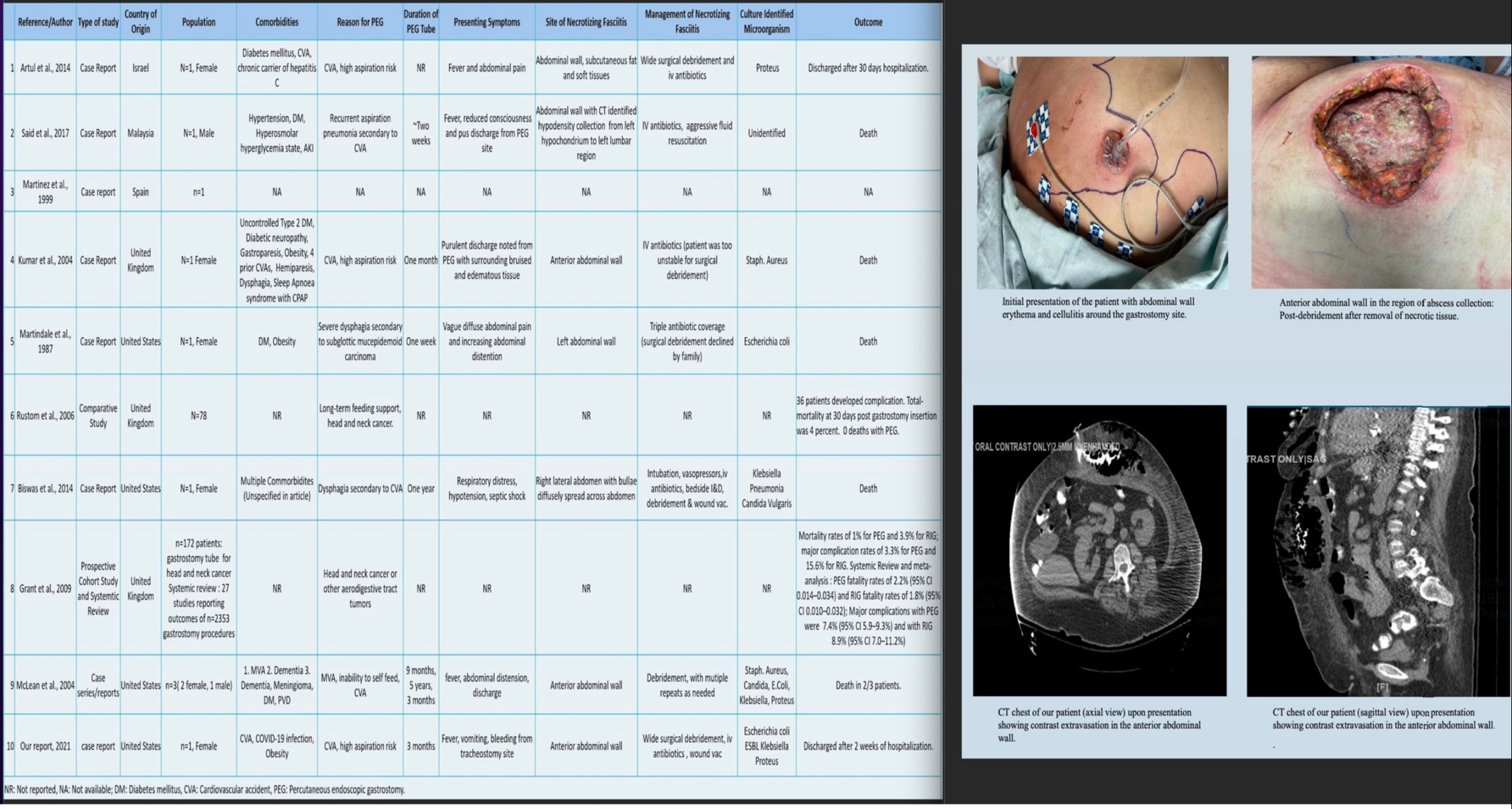
Figure: Review of Literature of all studies with percutaneous endoscopic gastrostomy associated necrotizing fasciitis of abdominal wall, along with images of abdominal wall necrotizing fasciitis in our patient, as described.
Disclosures:
Vishal Chandel indicated no relevant financial relationships.
Sridhar Reddy Patlolla indicated no relevant financial relationships.
Imran Khokhar indicated no relevant financial relationships.
Mathew Mathew indicated no relevant financial relationships.
Robin Zachariah indicated no relevant financial relationships.
Emad Mansoor indicated no relevant financial relationships.
Vishal Chandel, MD1, Sridhar Reddy Patlolla, MD1, Imran Khokhar, MD1, Mathew Mathew, MD1, Robin Zachariah, MD2, Emad Mansoor, MD3. B0716 - Abdominal Wall Necrotizing Fasciitis in a Recent COVID-19 Infection as a Rare Complication of Percutaneous Endoscopic Gastrostomy: Case Report and Review of Literature, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
