Back

Poster Session E - Tuesday Afternoon
Category: Esophagus
E0211 - Association Between Defective Secondary Peristalsis Detected by Functional Lumen Imaging Probe Topography (FLIP) and GERD
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio
Fangfang Wang, MD
Mayo Clinic Arizona
Phoenix, AZ
Presenting Author(s)
Fangfang Wang, MD1, Jennifer Horsley-Silva, MD2, Michael Crowell, PhD3, Marcelo F. Vela, MD3
1Mayo Clinic Arizona, Phoenix, AZ; 2Mayo Clinic Arizona, Scottsdale, AZ; 3Mayo Clinic, Scottsdale, AZ
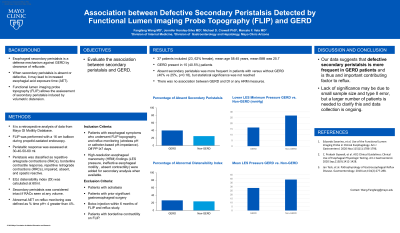
Introduction: Esophageal secondary peristalsis is a defense mechanism against GERD by clearance of refluxate. When absent or defective, it may lead to increased esophageal acid exposure time (AET). Functional lumen imaging probe topography (FLIP) allows assessment of secondary peristalsis induced by volumetric distension. Aim: evaluate the association between secondary peristalsis and GERD.
Methods: We included patients with esophageal symptoms who underwent FLIP topography and reflux monitoring (wireless pH or catheter-based pH-impedance) while off PPI ≥7 days, high-resolution esophageal manometry (HRM) findings (LES pressure, ineffective esophageal motility , absent contractility) were added for secondary analysis when available. Exclusion criteria: achalasia, prior gastroesophageal surgery, Botox injection within 6 months of FLIP and reflux study. Abnormal AET on reflux monitoring was defined as % time pH< 4 greater than 4%. FLIP was performed with a 16 cm balloon during propofol-sedated endoscopy; peristaltic response was assessed at 30-40-50-60 ml and classified as repetitive antegrade contractions (RACs), borderline contractile response, repetitive retrograde contractions (RRCs), impaired, absent, and spastic reactive. EGJ distensibility index (DI) was calculated at 60ml. Secondary peristalsis was considered intact if RACs seen at any volume, impaired otherwise. Those with borderline contractility but no RACs were excluded from analysis.. We assessed the association between FLIP and HRM findings and GERD by t test and chi square.
Results: 37 patients included (23, 62% female), mean age 58.45 years, mean BMI 25.7. GERD present in 15 (40.5%). Mean esophageal AET was lower in patients with versus without intact peristalsis but significance not reached (5.8% vs 3.0%, p=0.058). The proportion of patients with GERD was lower in patients with peristalsis versus without intact peristalsis but significance not reached (25% vs 40%, p=0.18). There was no association between GERD and DI or any HRM measures.
Discussion: Our data suggests that defective secondary peristalsis is more frequent in GERD patients and is thus and important contributing factor to reflux. Lack of significance may be due to small sample size and type II error, but a larger number of patients is needed to clarify this and data collection is ongoing.
Disclosures:
Fangfang Wang, MD1, Jennifer Horsley-Silva, MD2, Michael Crowell, PhD3, Marcelo F. Vela, MD3. E0211 - Association Between Defective Secondary Peristalsis Detected by Functional Lumen Imaging Probe Topography (FLIP) and GERD, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Mayo Clinic Arizona, Phoenix, AZ; 2Mayo Clinic Arizona, Scottsdale, AZ; 3Mayo Clinic, Scottsdale, AZ
Introduction: Esophageal secondary peristalsis is a defense mechanism against GERD by clearance of refluxate. When absent or defective, it may lead to increased esophageal acid exposure time (AET). Functional lumen imaging probe topography (FLIP) allows assessment of secondary peristalsis induced by volumetric distension. Aim: evaluate the association between secondary peristalsis and GERD.
Methods: We included patients with esophageal symptoms who underwent FLIP topography and reflux monitoring (wireless pH or catheter-based pH-impedance) while off PPI ≥7 days, high-resolution esophageal manometry (HRM) findings (LES pressure, ineffective esophageal motility , absent contractility) were added for secondary analysis when available. Exclusion criteria: achalasia, prior gastroesophageal surgery, Botox injection within 6 months of FLIP and reflux study. Abnormal AET on reflux monitoring was defined as % time pH< 4 greater than 4%. FLIP was performed with a 16 cm balloon during propofol-sedated endoscopy; peristaltic response was assessed at 30-40-50-60 ml and classified as repetitive antegrade contractions (RACs), borderline contractile response, repetitive retrograde contractions (RRCs), impaired, absent, and spastic reactive. EGJ distensibility index (DI) was calculated at 60ml. Secondary peristalsis was considered intact if RACs seen at any volume, impaired otherwise. Those with borderline contractility but no RACs were excluded from analysis.. We assessed the association between FLIP and HRM findings and GERD by t test and chi square.
Results: 37 patients included (23, 62% female), mean age 58.45 years, mean BMI 25.7. GERD present in 15 (40.5%). Mean esophageal AET was lower in patients with versus without intact peristalsis but significance not reached (5.8% vs 3.0%, p=0.058). The proportion of patients with GERD was lower in patients with peristalsis versus without intact peristalsis but significance not reached (25% vs 40%, p=0.18). There was no association between GERD and DI or any HRM measures.
Discussion: Our data suggests that defective secondary peristalsis is more frequent in GERD patients and is thus and important contributing factor to reflux. Lack of significance may be due to small sample size and type II error, but a larger number of patients is needed to clarify this and data collection is ongoing.
Disclosures:
Fangfang Wang indicated no relevant financial relationships.
Jennifer Horsley-Silva: Allakos – Clinical trial site. Celegene – Clinical trial site. Sanofi Genzyme / Regeneron – Clinical trial site. Sanofi Genzyme/Regeneron – Advisory Committee/Board Member.
Michael Crowell indicated no relevant financial relationships.
Marcelo Vela: Medtronic – Consultant.
Fangfang Wang, MD1, Jennifer Horsley-Silva, MD2, Michael Crowell, PhD3, Marcelo F. Vela, MD3. E0211 - Association Between Defective Secondary Peristalsis Detected by Functional Lumen Imaging Probe Topography (FLIP) and GERD, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
