Back

Poster Session B - Monday Morning
Category: Esophagus
B0256 - An Unusual Case of Dysphagia: Esophageal Squamous Cell Carcinoma From Untreated Achalasia
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Naima J. Hashi, MD
Mayo Clinic
Rochester, MN
Presenting Author(s)
Naima J. Hashi, MD, Babusai Rapaka, MD, Farah Abdul-Razzak, MD, Xiao Jing (Iris) Wang, MD
Mayo Clinic, Rochester, MN
Introduction: Achalasia leads to dysphagia due to impaired relaxation of the lower esophageal sphincter (LES). Evaluation of achalasia involves ruling out extrinsic compression from malignancies of the gastroesophageal junction, which produce similar clinical and radiologic findings. In rare instances, malignancy can be a consequence of achalasia itself. We present a case of esophageal squamous cell carcinoma (ESCC) from untreated achalasia of several decades’ duration.
Case Description/Methods: An 81-year-old female presented with progressive dysphagia. She described “trouble” with larger solid foods for years but reported worsening dysphagia to solids 6 months prior with progression to liquid dysphagia 3 months prior. She described the sensation as food getting lodged in the middle of her chest without odynophagia or difficulty initiating a swallow. She also had 100lb weight loss in these 6 months.
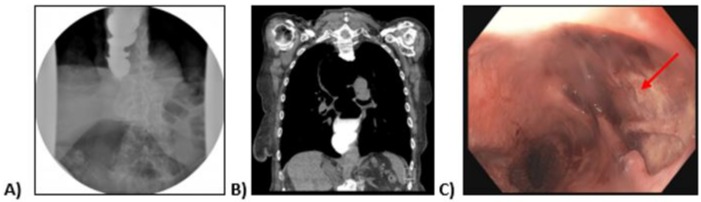
Patient underwent an esophagram showing marked dilatation of the distal esophagus with tapering distally concerning for achalasia (Figure 1A). Computed tomography of the chest showed marked dilatation of the esophagus, most severe proximally, with mass effect upon the mediastinum (Figure 1B). Esophagogastroduodenoscopy revealed a 5 cm large, cratered ulcer eroding through the esophagus (Figure 1C). Biopsies taken of the ulcer were consistent with ESCC.
Patient deferred further treatment of her malignancy and opted for hospice care.
Discussion: Achalasia is assumed to result from inflammatory degeneration of neurons of the esophagus. In addition to morbidity from dysphagia, achalasia increases patient risk of developing esophageal cancer up to 50-fold compared to the general population. Abnormal LES pressure leads to food stasis and promotes lactic acid production and fermentation due to bacterial overgrowth. This causes slow, continuous and chronic inflammation, damaging esophageal mucosa, and predisposing to dysplastic changes. Like our patient, patients with achalasia who develop cancer usually present with advanced disease, typically 20-25 years after symptom onset. Population studies are unclear if endoscopic screening is cost effective or reduces the risk of developing ESCC in patients with achalasia. However preliminary studies using exhaled volatile organic compounds and serum autoantibodies have demonstrated good specificity as noninvasive ways of screening for ESCC in these patients. Timely identification and treatment are needed to prevent progression to malignancy.
Disclosures:
Naima J. Hashi, MD, Babusai Rapaka, MD, Farah Abdul-Razzak, MD, Xiao Jing (Iris) Wang, MD. B0256 - An Unusual Case of Dysphagia: Esophageal Squamous Cell Carcinoma From Untreated Achalasia, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Mayo Clinic, Rochester, MN
Introduction: Achalasia leads to dysphagia due to impaired relaxation of the lower esophageal sphincter (LES). Evaluation of achalasia involves ruling out extrinsic compression from malignancies of the gastroesophageal junction, which produce similar clinical and radiologic findings. In rare instances, malignancy can be a consequence of achalasia itself. We present a case of esophageal squamous cell carcinoma (ESCC) from untreated achalasia of several decades’ duration.
Case Description/Methods: An 81-year-old female presented with progressive dysphagia. She described “trouble” with larger solid foods for years but reported worsening dysphagia to solids 6 months prior with progression to liquid dysphagia 3 months prior. She described the sensation as food getting lodged in the middle of her chest without odynophagia or difficulty initiating a swallow. She also had 100lb weight loss in these 6 months.
Patient underwent an esophagram showing marked dilatation of the distal esophagus with tapering distally concerning for achalasia (Figure 1A). Computed tomography of the chest showed marked dilatation of the esophagus, most severe proximally, with mass effect upon the mediastinum (Figure 1B). Esophagogastroduodenoscopy revealed a 5 cm large, cratered ulcer eroding through the esophagus (Figure 1C). Biopsies taken of the ulcer were consistent with ESCC.
Patient deferred further treatment of her malignancy and opted for hospice care.
Discussion: Achalasia is assumed to result from inflammatory degeneration of neurons of the esophagus. In addition to morbidity from dysphagia, achalasia increases patient risk of developing esophageal cancer up to 50-fold compared to the general population. Abnormal LES pressure leads to food stasis and promotes lactic acid production and fermentation due to bacterial overgrowth. This causes slow, continuous and chronic inflammation, damaging esophageal mucosa, and predisposing to dysplastic changes. Like our patient, patients with achalasia who develop cancer usually present with advanced disease, typically 20-25 years after symptom onset. Population studies are unclear if endoscopic screening is cost effective or reduces the risk of developing ESCC in patients with achalasia. However preliminary studies using exhaled volatile organic compounds and serum autoantibodies have demonstrated good specificity as noninvasive ways of screening for ESCC in these patients. Timely identification and treatment are needed to prevent progression to malignancy.
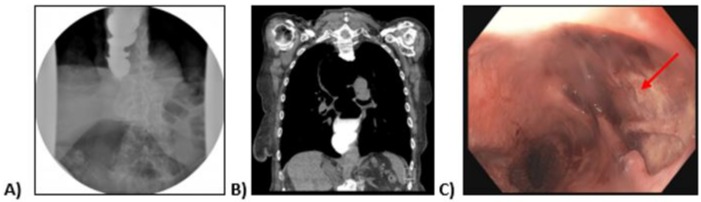
Figure: Figure 1: A) Esophagram showing marked dilatation of the distal esophagus with slight tapering distally. B) Computed tomography of the chest without contrast showing marked dilatation of the esophagus, most severe proximally, with mass effect upon the mediastinum. C) Esophagogastroduodenoscopy revealing a 5 cm large, cratered ulcer eroding through the esophagus (red arrow).
Disclosures:
Naima Hashi indicated no relevant financial relationships.
Babusai Rapaka indicated no relevant financial relationships.
Farah Abdul-Razzak indicated no relevant financial relationships.
Xiao Jing (Iris) Wang indicated no relevant financial relationships.
Naima J. Hashi, MD, Babusai Rapaka, MD, Farah Abdul-Razzak, MD, Xiao Jing (Iris) Wang, MD. B0256 - An Unusual Case of Dysphagia: Esophageal Squamous Cell Carcinoma From Untreated Achalasia, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
