Back
Poster Session E - Tuesday Afternoon
Category: Esophagus
E0228 - Tracheoesophageal Fistula Presenting With Gastrostomy Tube Pressurization
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
- AB
Andreas W. Bub, MD
Stamford Hospital
Stamford, Connecticut
Presenting Author(s)
Andreas W. Bub, MD1, Robert Dettmer, MD2, Michael I. Ebright, MD3, Frantz Hastrup, MD1
1Stamford Hospital, Stamford, CT; 2Gastroenterology Hepatology Associates, Stamford, CT; 3Columbia University Medical Center, Stamford, CT
Introduction: Patients with COVID pneumonia who require intubation and prolonged mechanical ventilation are at risk for complications such as recurrent infection, tracheomalacia, tracheal stenosis, and the development of tracheoesophageal fistula (TEF). TEF is a devastating complication where the trachea and esophagus develop an abnormal connection in the lower airway that dramatically increases the mortality of critically ill patients by recurrent aspiration and pneumonias. Though commonly associated with neoplasms another risk is pressure induced ischemia of the common wall between the trachea and esophagus. This can occur due to overinflation of the endotracheal (ET) cuff, especially with concomitant use of a nasogastric tube (NGT). Definitive management requires surgical repair.
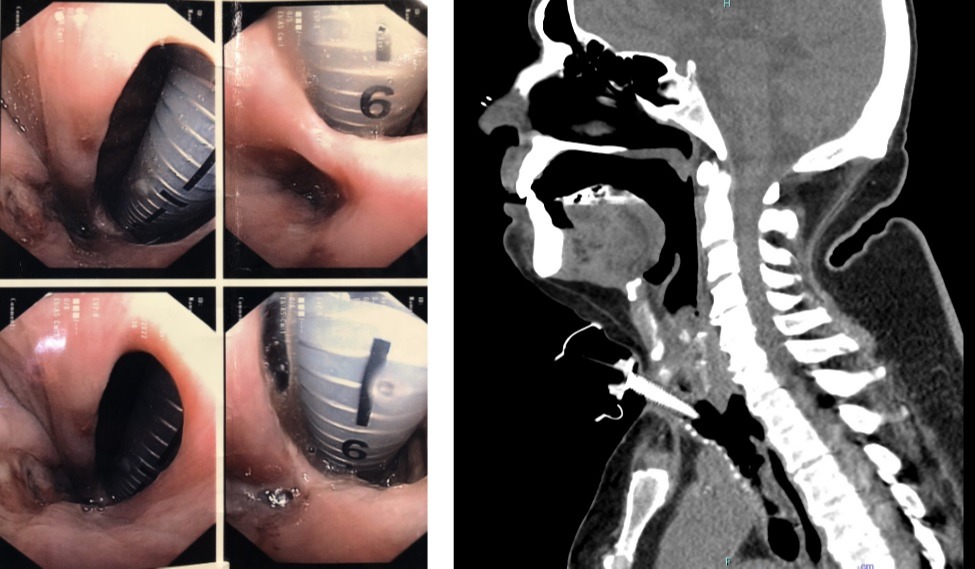
Case Description/Methods: A 69 year-old male patient presented with acute hypoxemic respiratory failure secondary to COVID pneumonia requiring intubation and insertion of an NGT. On day 29 the patient underwent percutaneous enterogastrostomy (PEG) placement and tracheostomy; it was noted intraoperatively that the tracheal mucosa was inflamed and friable. On day 36 bronchoscopy was performed through the tracheostomy tube due to concerns for mucus plugging. Friable mucosa with granulation tissue was seen at the distal end of the tube, so an extra-long tracheostomy tube was exchanged to bypass the granulation tissue. Later that night the ventilator measured a 50% discrepancy between the delivered and exhaled tidal volumes, triggering an alarm. Exam noted distension of the PEG-bag with a fluid meniscus in the tubing moving in sync with each respiration. TEF was considered and bronchoscopic evaluation confirmed a 1 centimeter TEF. The patient underwent successful TEF repair and is slowly recovering.
Discussion: Critically ill patients who require prolonged support are at high risk of complications and device related injury. With each device-day there is an increased risk of complications, such as infection, dislodgement, and pressure-related injuries. This case highlights the importance of serial physical examinations as well as understanding possible device related complications. An unexpected finding, such as a persistent air leak, air in a PEG bag, or a fluctuating meniscus should raise suspicion for the development of a serious complication and would warrant prompt confirmatory testing. Our literature review revealed no reports of a PEG tube abnormalities as a presenting finding for TEF.
Disclosures:
Andreas W. Bub, MD1, Robert Dettmer, MD2, Michael I. Ebright, MD3, Frantz Hastrup, MD1. E0228 - Tracheoesophageal Fistula Presenting With Gastrostomy Tube Pressurization, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Stamford Hospital, Stamford, CT; 2Gastroenterology Hepatology Associates, Stamford, CT; 3Columbia University Medical Center, Stamford, CT
Introduction: Patients with COVID pneumonia who require intubation and prolonged mechanical ventilation are at risk for complications such as recurrent infection, tracheomalacia, tracheal stenosis, and the development of tracheoesophageal fistula (TEF). TEF is a devastating complication where the trachea and esophagus develop an abnormal connection in the lower airway that dramatically increases the mortality of critically ill patients by recurrent aspiration and pneumonias. Though commonly associated with neoplasms another risk is pressure induced ischemia of the common wall between the trachea and esophagus. This can occur due to overinflation of the endotracheal (ET) cuff, especially with concomitant use of a nasogastric tube (NGT). Definitive management requires surgical repair.
Case Description/Methods: A 69 year-old male patient presented with acute hypoxemic respiratory failure secondary to COVID pneumonia requiring intubation and insertion of an NGT. On day 29 the patient underwent percutaneous enterogastrostomy (PEG) placement and tracheostomy; it was noted intraoperatively that the tracheal mucosa was inflamed and friable. On day 36 bronchoscopy was performed through the tracheostomy tube due to concerns for mucus plugging. Friable mucosa with granulation tissue was seen at the distal end of the tube, so an extra-long tracheostomy tube was exchanged to bypass the granulation tissue. Later that night the ventilator measured a 50% discrepancy between the delivered and exhaled tidal volumes, triggering an alarm. Exam noted distension of the PEG-bag with a fluid meniscus in the tubing moving in sync with each respiration. TEF was considered and bronchoscopic evaluation confirmed a 1 centimeter TEF. The patient underwent successful TEF repair and is slowly recovering.
Discussion: Critically ill patients who require prolonged support are at high risk of complications and device related injury. With each device-day there is an increased risk of complications, such as infection, dislodgement, and pressure-related injuries. This case highlights the importance of serial physical examinations as well as understanding possible device related complications. An unexpected finding, such as a persistent air leak, air in a PEG bag, or a fluctuating meniscus should raise suspicion for the development of a serious complication and would warrant prompt confirmatory testing. Our literature review revealed no reports of a PEG tube abnormalities as a presenting finding for TEF.
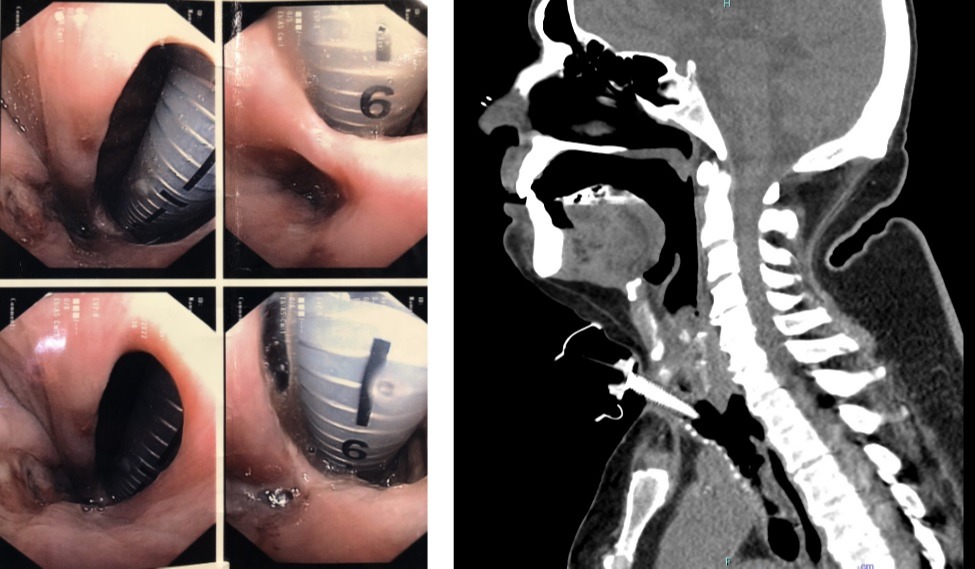
Figure: Left: TEF as visualized from the esophagus during endoscopy. ET tube visible through TEF.
Right: Neck CT showing the connection between the Esophagus and Trachea
Right: Neck CT showing the connection between the Esophagus and Trachea
Disclosures:
Andreas Bub indicated no relevant financial relationships.
Robert Dettmer indicated no relevant financial relationships.
Michael Ebright: Medtronic – Consultant.
Frantz Hastrup indicated no relevant financial relationships.
Andreas W. Bub, MD1, Robert Dettmer, MD2, Michael I. Ebright, MD3, Frantz Hastrup, MD1. E0228 - Tracheoesophageal Fistula Presenting With Gastrostomy Tube Pressurization, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
