Back

Poster Session E - Tuesday Afternoon
Category: Esophagus
E0230 - Lymphocytic Esophagitis: A Rare Etiology for Persistent Heartburn
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Mahmoud Bayoumi, MD, MPH
University of Arizona College of Medicine
Phoenix, AZ
Presenting Author(s)
Mahmoud Bayoumi, MD, MPH1, Megan B. Ghai, MD, MPH, MA1, Kelli Kosako Yost, MD1, Wesley A. Robertson, MD, MPH, MPA1, Dayna Telken, DO1, David Drewitz, MD2
1University of Arizona College of Medicine, Phoenix, AZ; 2Arizona Digestive Health, Phoenix, AZ
Introduction: Lymphocytic esophagitis (LE) is a relatively newly recognized and emerging condition. It has a higher predominance in females and is highly associated with inflammatory bowel disease and smoking. Dysphagia and heartburn are the two most common presentations. The esophagus usually appears normal by endoscopy; however, esophageal rings, webs, nodularities, furrows, and strictures have been described. Presented is a case with persistent heartburn and epigastric discomfort found to have LE with an unusual response to therapy.
Case Description/Methods: A 24-year-old female with a history of ulcerative colitis (UC) and tobacco use came for esophagogastroduodenoscopy (EGD) due to constant heartburn and epigastric abdominal discomfort that started two months ago. She has been prescribed Omeprazole twice daily with no adequate response. Her UC was well controlled on infliximab with normal inflammatory markers.
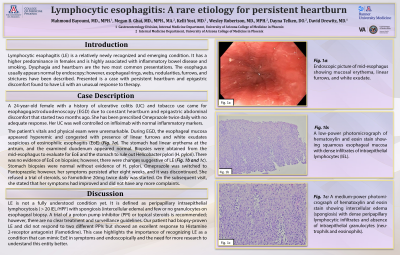
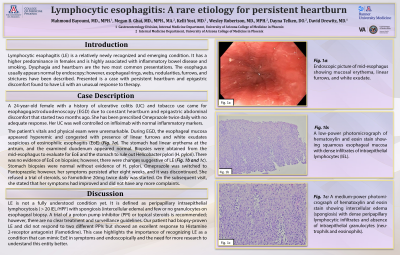
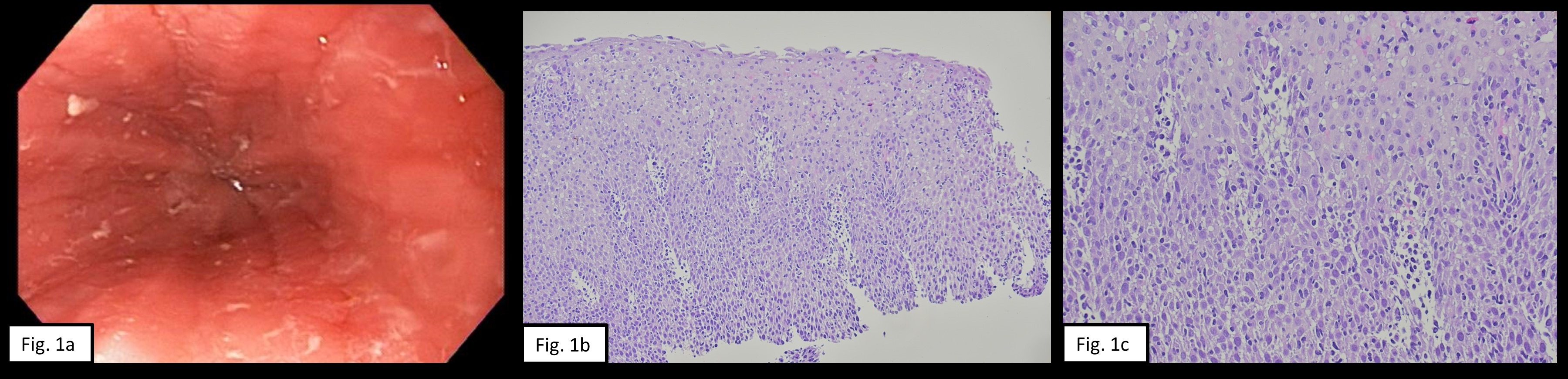
The patient's vitals and physical exam were unremarkable. During EGD, the esophageal mucosa appeared hyperemic and congested with presence of linear furrows and white exudates suspicious of eosinophilic esophagitis (EoE) (Fig. 1a). The stomach had linear erythema at the antrum, and the examined duodenum appeared normal. Biopsies were obtained from the mid-esophagus to evaluate for EoE and the stomach to rule out Helicobacter pylori (H. pylori). There was no evidence of EoE on biopsies; however, there were changes suggestive of LE (Fig. 1b and 1c). Stomach biopsies were normal without evidence of H. pylori. Omeprazole was switched to Pantoprazole; however, her symptoms persisted after eight weeks, and it was discontinued. She refused a trial of steroids, so Famotidine 20mg twice daily was started. On the subsequent visit, she stated that her symptoms had improved and did not have any more complaints.
Discussion: LE is not a fully understood condition yet. It is defined as peripapillary intraepithelial lymphocytosis ( > 20 IEL/HPF) with spongiosis (intercellular edema) and few or no granulocytes on esophageal biopsy. A trial of a proton pump inhibitor (PPI) or topical steroids is recommended; however, there are no clear treatment and surveillance guidelines. Our patient had biopsy-proven LE and did not respond to two different PPIs but showed an excellent response to Histamine 2-receptor antagonist (Famotidine). This case highlights the importance of recognizing LE as a condition that can mimic EoE in symptoms and endoscopically and the need for more research to understand this entity better.
Disclosures:
Mahmoud Bayoumi, MD, MPH1, Megan B. Ghai, MD, MPH, MA1, Kelli Kosako Yost, MD1, Wesley A. Robertson, MD, MPH, MPA1, Dayna Telken, DO1, David Drewitz, MD2. E0230 - Lymphocytic Esophagitis: A Rare Etiology for Persistent Heartburn, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Arizona College of Medicine, Phoenix, AZ; 2Arizona Digestive Health, Phoenix, AZ
Introduction: Lymphocytic esophagitis (LE) is a relatively newly recognized and emerging condition. It has a higher predominance in females and is highly associated with inflammatory bowel disease and smoking. Dysphagia and heartburn are the two most common presentations. The esophagus usually appears normal by endoscopy; however, esophageal rings, webs, nodularities, furrows, and strictures have been described. Presented is a case with persistent heartburn and epigastric discomfort found to have LE with an unusual response to therapy.
Case Description/Methods: A 24-year-old female with a history of ulcerative colitis (UC) and tobacco use came for esophagogastroduodenoscopy (EGD) due to constant heartburn and epigastric abdominal discomfort that started two months ago. She has been prescribed Omeprazole twice daily with no adequate response. Her UC was well controlled on infliximab with normal inflammatory markers.
The patient's vitals and physical exam were unremarkable. During EGD, the esophageal mucosa appeared hyperemic and congested with presence of linear furrows and white exudates suspicious of eosinophilic esophagitis (EoE) (Fig. 1a). The stomach had linear erythema at the antrum, and the examined duodenum appeared normal. Biopsies were obtained from the mid-esophagus to evaluate for EoE and the stomach to rule out Helicobacter pylori (H. pylori). There was no evidence of EoE on biopsies; however, there were changes suggestive of LE (Fig. 1b and 1c). Stomach biopsies were normal without evidence of H. pylori. Omeprazole was switched to Pantoprazole; however, her symptoms persisted after eight weeks, and it was discontinued. She refused a trial of steroids, so Famotidine 20mg twice daily was started. On the subsequent visit, she stated that her symptoms had improved and did not have any more complaints.
Discussion: LE is not a fully understood condition yet. It is defined as peripapillary intraepithelial lymphocytosis ( > 20 IEL/HPF) with spongiosis (intercellular edema) and few or no granulocytes on esophageal biopsy. A trial of a proton pump inhibitor (PPI) or topical steroids is recommended; however, there are no clear treatment and surveillance guidelines. Our patient had biopsy-proven LE and did not respond to two different PPIs but showed an excellent response to Histamine 2-receptor antagonist (Famotidine). This case highlights the importance of recognizing LE as a condition that can mimic EoE in symptoms and endoscopically and the need for more research to understand this entity better.
Figure: Fig. 1a: Endoscopic picture of mid-esophagus showing mucosal erythema, linear furrows, and white exudate.
Fig. 1b: A low-power photomicrograph of hematoxylin and eosin stain showing squamous esophageal mucosa with dense infiltrates of intraepithelial lymphocytes (IEL).
Fig. 1c: A medium-power photomicrograph of hematoxylin and eosin stain showing intercellular edema (spongiosis) with dense peripapillary lymphocytic infiltrates and absence of intraepithelial granulocytes (neutrophils and eosinophils).
Fig. 1b: A low-power photomicrograph of hematoxylin and eosin stain showing squamous esophageal mucosa with dense infiltrates of intraepithelial lymphocytes (IEL).
Fig. 1c: A medium-power photomicrograph of hematoxylin and eosin stain showing intercellular edema (spongiosis) with dense peripapillary lymphocytic infiltrates and absence of intraepithelial granulocytes (neutrophils and eosinophils).
Disclosures:
Mahmoud Bayoumi indicated no relevant financial relationships.
Megan Ghai indicated no relevant financial relationships.
Kelli Kosako Yost indicated no relevant financial relationships.
Wesley Robertson indicated no relevant financial relationships.
Dayna Telken indicated no relevant financial relationships.
David Drewitz indicated no relevant financial relationships.
Mahmoud Bayoumi, MD, MPH1, Megan B. Ghai, MD, MPH, MA1, Kelli Kosako Yost, MD1, Wesley A. Robertson, MD, MPH, MPA1, Dayna Telken, DO1, David Drewitz, MD2. E0230 - Lymphocytic Esophagitis: A Rare Etiology for Persistent Heartburn, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
