Back

Poster Session E - Tuesday Afternoon
Category: Esophagus
E0235 - A Case of Esophagitis in a Patient With Poorly Controlled Systemic Lupus Erythematosus
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio
- CP
Colton Pence, MD
New York-Presbyterian Hospital/Weill Cornell Medicine
New York, NY
Presenting Author(s)
Colton Pence, MD, Preston Atteberry, MD, David Wan, MD
New York-Presbyterian Hospital/Weill Cornell Medicine, New York, NY
Introduction: Primary Systemic Lupus Erythematosus (SLE) esophagitis is a rare entity that most commonly presents with odynophagia and dysphagia. Though esophageal involvement with SLE is common, it typically manifests as a motility disorder or secondary infectious or pill esophagitis rather than a primary SLE esophagitis. While its underlying pathologic mechanisms may be similar to other manifestations of SLE, SLE esophagitis remains poorly understood.
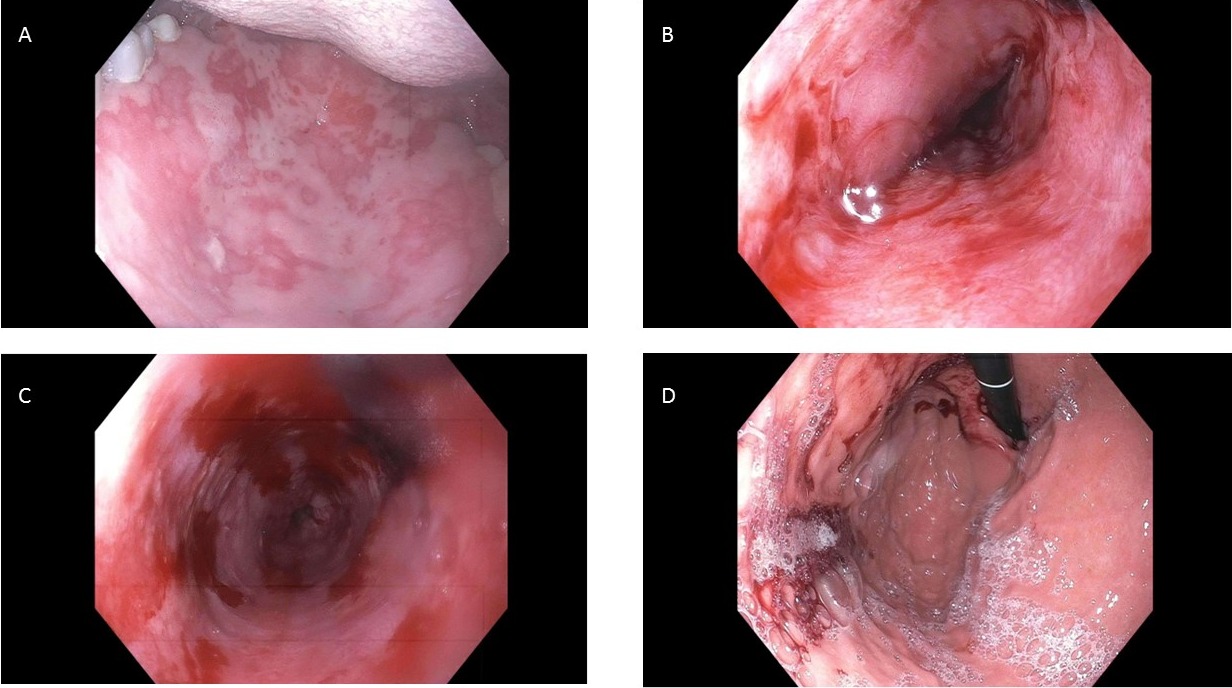
Case Description/Methods: A 33-year-old man with history of juvenile discoid SLE complicated by arthritis, cutaneous involvement, oral ulcers, cerebritis, and four-limb avascular necrosis secondary to chronic steroid use presented with a week of worsening oral ulcers, new-onset odynophagia, stable diffuse arthralgias, and active discoid lupus with ear and scalp involvement. His oral ulcers were more numerous and painful than was typical for his flares, and he had not previously experienced odynophagia during flares. Esophagogastroduodenoscopy (EGD) revealed diffuse erythematous, exudative, sloughed mucosa throughout the entire esophagus and stomach, while initial pathology revealed nonspecific findings with concern for possible vesiculobullous disorder. The patient was managed with increased immunosuppression for presumed SLE flare and his symptoms improved. Repeat EGD was performed to rule out an autoimmune blistering process, and immunofluorescence demonstrated granular deposits of IgG, IgM, and complement within the epithelial basement membrane, suggestive of SLE as the basis for the esophageal inflammation.
Discussion: SLE esophagitis is an uncommon condition that results from granular deposition of immune complexes in the basement membrane of the esophageal epithelium, representing a form of SLE mucositis in an unusual location. In patients with a history of SLE who present with odynophagia or dysphagia this diagnosis should be considered as a possibility, especially in those with many previous SLE-related complications. Diagnosis requires EGD with biopsy to differentiate between this and more common causes of esophagitis seen in SLE patients. Management of SLE esophagitis should mirror treatment of other SLE flares with appropriate immunosuppressive therapy but warrants follow-up with a gastroenterologist to assess need for future EGD monitoring.
Disclosures:
Colton Pence, MD, Preston Atteberry, MD, David Wan, MD. E0235 - A Case of Esophagitis in a Patient With Poorly Controlled Systemic Lupus Erythematosus, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
New York-Presbyterian Hospital/Weill Cornell Medicine, New York, NY
Introduction: Primary Systemic Lupus Erythematosus (SLE) esophagitis is a rare entity that most commonly presents with odynophagia and dysphagia. Though esophageal involvement with SLE is common, it typically manifests as a motility disorder or secondary infectious or pill esophagitis rather than a primary SLE esophagitis. While its underlying pathologic mechanisms may be similar to other manifestations of SLE, SLE esophagitis remains poorly understood.
Case Description/Methods: A 33-year-old man with history of juvenile discoid SLE complicated by arthritis, cutaneous involvement, oral ulcers, cerebritis, and four-limb avascular necrosis secondary to chronic steroid use presented with a week of worsening oral ulcers, new-onset odynophagia, stable diffuse arthralgias, and active discoid lupus with ear and scalp involvement. His oral ulcers were more numerous and painful than was typical for his flares, and he had not previously experienced odynophagia during flares. Esophagogastroduodenoscopy (EGD) revealed diffuse erythematous, exudative, sloughed mucosa throughout the entire esophagus and stomach, while initial pathology revealed nonspecific findings with concern for possible vesiculobullous disorder. The patient was managed with increased immunosuppression for presumed SLE flare and his symptoms improved. Repeat EGD was performed to rule out an autoimmune blistering process, and immunofluorescence demonstrated granular deposits of IgG, IgM, and complement within the epithelial basement membrane, suggestive of SLE as the basis for the esophageal inflammation.
Discussion: SLE esophagitis is an uncommon condition that results from granular deposition of immune complexes in the basement membrane of the esophageal epithelium, representing a form of SLE mucositis in an unusual location. In patients with a history of SLE who present with odynophagia or dysphagia this diagnosis should be considered as a possibility, especially in those with many previous SLE-related complications. Diagnosis requires EGD with biopsy to differentiate between this and more common causes of esophagitis seen in SLE patients. Management of SLE esophagitis should mirror treatment of other SLE flares with appropriate immunosuppressive therapy but warrants follow-up with a gastroenterologist to assess need for future EGD monitoring.
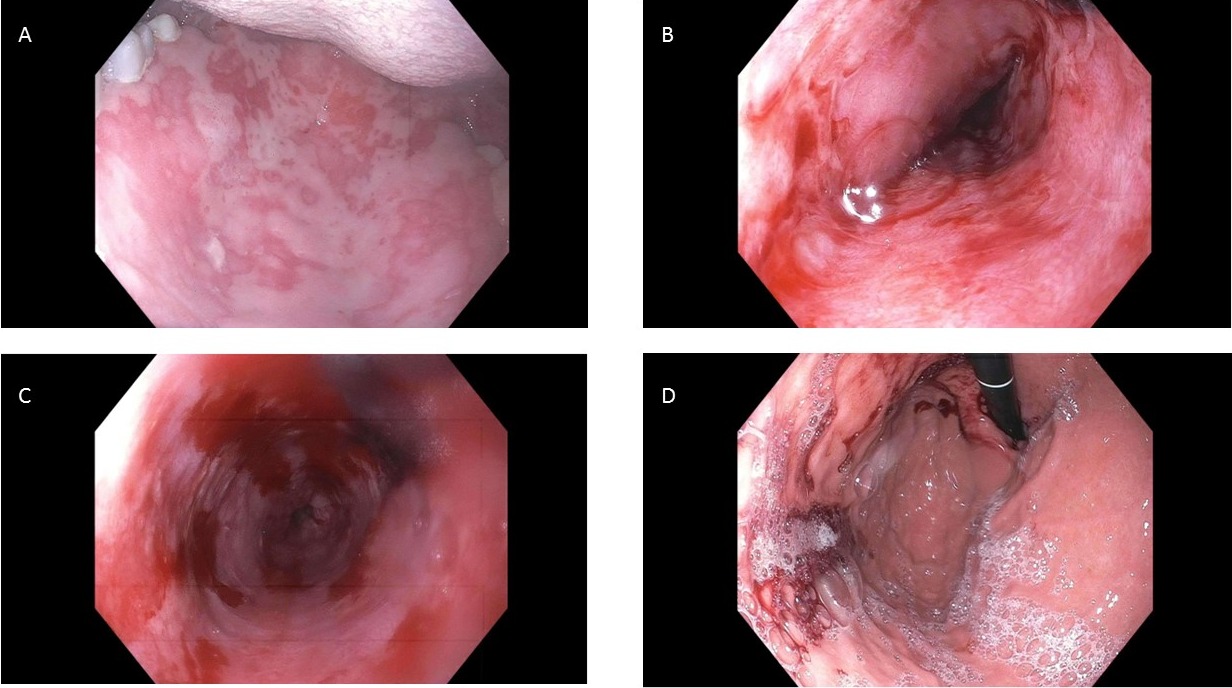
Figure: Figure 1: A: Ulcers on palate of mouth; B: Middle third of the esophagus; C: Lower third of the esophagus; D: Antrum of the stomach
Disclosures:
Colton Pence indicated no relevant financial relationships.
Preston Atteberry indicated no relevant financial relationships.
David Wan indicated no relevant financial relationships.
Colton Pence, MD, Preston Atteberry, MD, David Wan, MD. E0235 - A Case of Esophagitis in a Patient With Poorly Controlled Systemic Lupus Erythematosus, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
