Back

Poster Session D - Tuesday Morning
Category: Interventional Endoscopy
D0457 - Stones, Strictures and Atrophy: Treating Sequelae of Infectious Hepatolithiasis
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
Jason Stibbe, MD, MS
LSUHSC
New Orleans, LA
Presenting Author(s)
Jason Stibbe, MD, MS, Stephen Landreneau, MD
LSUHSC, New Orleans, LA
Introduction: Primary intrahepatic cholelithiasis has been well-associated with brown or pigmented stones and recurrent pyogenic cholangitis. However, other important potential chronic complications exist beyond cholangitis of which gastroenterologists should be aware.
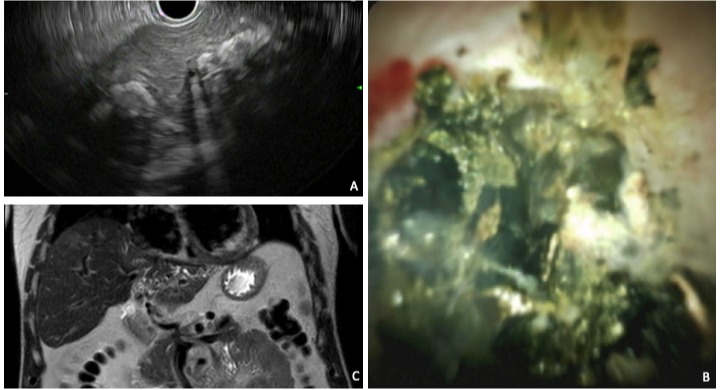
Case Description/Methods: We present a case of a 57 year-old man with history of diabetes who returned from a 13-month stay in Japan to be admitted to an outside facility with DKA and cholangitis. He was found to have a liver abscess and left hepatic duct stricture treated with sphincterotomy, biliary stenting via ERCP, abscess drainage, and cholecystectomy. He followed up externally for stent removal with normalization of liver chemistries however CT imaging 1 year later showed persistent left hepatic duct stricture with intrahepatic segmental dilation. He experienced no early satiety, weight loss, or jaundice. He was referred to our service for further evaluation of chronic indeterminate biliary stricture. Endoscopic ultrasound demonstrated extensive small and large left-sided hepatolithiasis (A). Cholangiography during ERCP demonstrated complete filling defect of the left intrahepatic biliary ductal system preventing selective guidewire passage. Cholangioscopy was performed with successful electrohydraulic lithotripsy (EHL) of stone burden in the left main hepatic system for selective wire passage and stenting of the left intrahepatic system with a plastic stent. Biliary epithelium appeared smooth and benign. The patient was given antibiotics with no complications. ERCP was repeated in 6 weeks with further cholangioscopy with EHL fragmentation and removal of stones in left intrahepatic ductal branches, however ductal disease remained throughout smaller distal branches of the left lobe on cholangiogram. The main duct was protected with a fully-covered metal stent and antibiotics were given. Follow-up MRI/MRCP demonstrated atrophic left liver lobe (C) in addition to our findings. Left partial hepatectomy was thus performed by Surgery for definitive therapy of the diseased lobe and the patient did well post-operatively with benign pathology.
Discussion: Even in the absence of a typical recurrent cholangitis clinical syndrome, treatment of other chronic sequelae of severe primary hepatolithiasis is important in the prevention of progression to cirrhosis. Multiple interventional endoscopic methods are available and should be utilized to establish the diagnosis and optimize therapy; which may include surgery in severe cases.
Disclosures:
Jason Stibbe, MD, MS, Stephen Landreneau, MD. D0457 - Stones, Strictures and Atrophy: Treating Sequelae of Infectious Hepatolithiasis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
LSUHSC, New Orleans, LA
Introduction: Primary intrahepatic cholelithiasis has been well-associated with brown or pigmented stones and recurrent pyogenic cholangitis. However, other important potential chronic complications exist beyond cholangitis of which gastroenterologists should be aware.
Case Description/Methods: We present a case of a 57 year-old man with history of diabetes who returned from a 13-month stay in Japan to be admitted to an outside facility with DKA and cholangitis. He was found to have a liver abscess and left hepatic duct stricture treated with sphincterotomy, biliary stenting via ERCP, abscess drainage, and cholecystectomy. He followed up externally for stent removal with normalization of liver chemistries however CT imaging 1 year later showed persistent left hepatic duct stricture with intrahepatic segmental dilation. He experienced no early satiety, weight loss, or jaundice. He was referred to our service for further evaluation of chronic indeterminate biliary stricture. Endoscopic ultrasound demonstrated extensive small and large left-sided hepatolithiasis (A). Cholangiography during ERCP demonstrated complete filling defect of the left intrahepatic biliary ductal system preventing selective guidewire passage. Cholangioscopy was performed with successful electrohydraulic lithotripsy (EHL) of stone burden in the left main hepatic system for selective wire passage and stenting of the left intrahepatic system with a plastic stent. Biliary epithelium appeared smooth and benign. The patient was given antibiotics with no complications. ERCP was repeated in 6 weeks with further cholangioscopy with EHL fragmentation and removal of stones in left intrahepatic ductal branches, however ductal disease remained throughout smaller distal branches of the left lobe on cholangiogram. The main duct was protected with a fully-covered metal stent and antibiotics were given. Follow-up MRI/MRCP demonstrated atrophic left liver lobe (C) in addition to our findings. Left partial hepatectomy was thus performed by Surgery for definitive therapy of the diseased lobe and the patient did well post-operatively with benign pathology.
Discussion: Even in the absence of a typical recurrent cholangitis clinical syndrome, treatment of other chronic sequelae of severe primary hepatolithiasis is important in the prevention of progression to cirrhosis. Multiple interventional endoscopic methods are available and should be utilized to establish the diagnosis and optimize therapy; which may include surgery in severe cases.
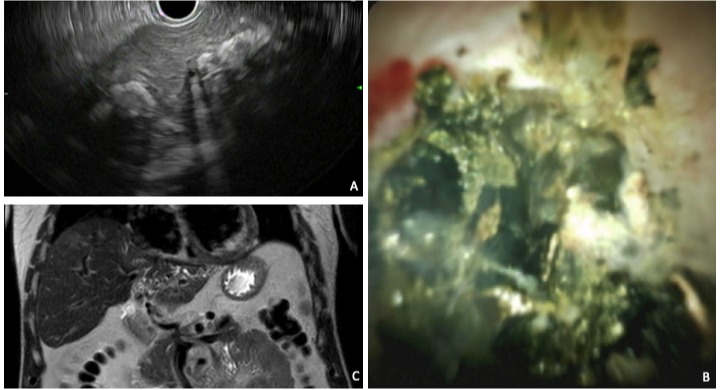
Figure: (A) Linear EUS view of left lobe intrahepatic cholelithiasis; (B) cholangioscopic view of intrahepatic cholelithiasis fragmented by electrohydraulic lithotripsy; (C) MRI with left lobe atrophy and hepatolithiasis.
Disclosures:
Jason Stibbe indicated no relevant financial relationships.
Stephen Landreneau indicated no relevant financial relationships.
Jason Stibbe, MD, MS, Stephen Landreneau, MD. D0457 - Stones, Strictures and Atrophy: Treating Sequelae of Infectious Hepatolithiasis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

