Back

Poster Session B - Monday Morning
Category: Functional Bowel Disease
B0276 - Stop, Drop, and Roll: One Woman’s Pelvic Floor Disease Journey
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

David Lehoang, MD, MBA
Keck School of Medicine, University of Southern California
Los Angeles, CA
Presenting Author(s)
David Lehoang, MD, MBA, Sean Dewberry, , Niharika Mallepally, MD, MPH, Christine Hsieh, MD, Sonia Sharma, MD
Keck School of Medicine, University of Southern California, Los Angeles, CA
Introduction: Pelvic floor disease includes symptoms of the anterior (urinary, vaginal) and posterior (anorectal) pelvic floor. This case describes a woman who developed dyssynergic defecation after surgical management of urinary incontinence. The diagnostic route taken to reveal the unusual cause of her symptoms is a lesson in how to evaluate ambiguous gastrointestinal(GI)/genitourinary symptoms.
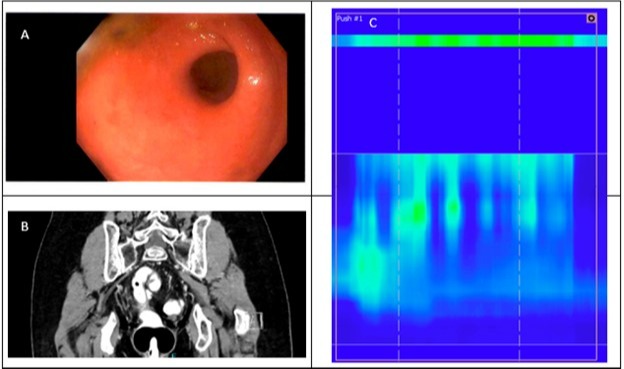
Case Description/Methods: A 69-year-old woman presents with bloating and difficulty defecating for 2 years. She senses incomplete evacuation, passing 1-2 thin stools per day despite an extensive bowel regimen (e.g. posturing, straining). Two years ago, she underwent sacrocolpopexy and mesh placement to treat pelvic organ prolapse. Her urinary incontinence improved but constipation worsened. She was thus evaluated by GI- many CTs showed nonspecific sigmoid (SC) thickening. A colonoscopy noted SC narrowing; mucosa pathology was normal. She came to our clinic to investigate further. Digital rectal exam had a normal tone with widening of the vault with strain. Anorectal manometry (ARM) showed dyssynergic defecation and unsuccessful balloon expulsion, consistent with mechanical obstruction. A flexible sigmoidoscopy showed benign-appearing extrinsic compression at the rectosigmoid junction. The SC also had a large stool burden despite 2 pre-procedure enemas. Given a concern for mass effect of the mesh into the colon, an exploratory laparoscopy was performed, showing a redundant SC with scarred, edematous mesentery. A partial sigmoidectomy was performed and adhesions at the anterior rectal wall (near the sacrocolpopexy mesh) were lysed. In just 3 months, the patient’s symptoms resolved. Repeat ARM had a normal defecation pattern and balloon expulsion.
Discussion: Postoperative adhesions are present after 63-97% of open abdominal surgeries. The most common complication of such adhesions is bowel obstruction, occurring in 15% of patients within 1 month of surgery. Our patient had an even more unique complication- constipation and dyssynergic defecation. Literature on post-op adhesions and defecation dysfunction mainly describes surgery of the rectal sphincter. In contrast, the sacrocolpopexy did not involve the rectum or surrounding peritoneum, but caused adhesions with a mass effect on the rectum. Given the morbidity associated with lower abdominal adhesions, suspicion must remain high in populations with a history of complicated abdominal surgery- especially for treatment of anterior pelvic floor disease.
Disclosures:
David Lehoang, MD, MBA, Sean Dewberry, , Niharika Mallepally, MD, MPH, Christine Hsieh, MD, Sonia Sharma, MD. B0276 - Stop, Drop, and Roll: One Woman’s Pelvic Floor Disease Journey, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Keck School of Medicine, University of Southern California, Los Angeles, CA
Introduction: Pelvic floor disease includes symptoms of the anterior (urinary, vaginal) and posterior (anorectal) pelvic floor. This case describes a woman who developed dyssynergic defecation after surgical management of urinary incontinence. The diagnostic route taken to reveal the unusual cause of her symptoms is a lesson in how to evaluate ambiguous gastrointestinal(GI)/genitourinary symptoms.
Case Description/Methods: A 69-year-old woman presents with bloating and difficulty defecating for 2 years. She senses incomplete evacuation, passing 1-2 thin stools per day despite an extensive bowel regimen (e.g. posturing, straining). Two years ago, she underwent sacrocolpopexy and mesh placement to treat pelvic organ prolapse. Her urinary incontinence improved but constipation worsened. She was thus evaluated by GI- many CTs showed nonspecific sigmoid (SC) thickening. A colonoscopy noted SC narrowing; mucosa pathology was normal. She came to our clinic to investigate further. Digital rectal exam had a normal tone with widening of the vault with strain. Anorectal manometry (ARM) showed dyssynergic defecation and unsuccessful balloon expulsion, consistent with mechanical obstruction. A flexible sigmoidoscopy showed benign-appearing extrinsic compression at the rectosigmoid junction. The SC also had a large stool burden despite 2 pre-procedure enemas. Given a concern for mass effect of the mesh into the colon, an exploratory laparoscopy was performed, showing a redundant SC with scarred, edematous mesentery. A partial sigmoidectomy was performed and adhesions at the anterior rectal wall (near the sacrocolpopexy mesh) were lysed. In just 3 months, the patient’s symptoms resolved. Repeat ARM had a normal defecation pattern and balloon expulsion.
Discussion: Postoperative adhesions are present after 63-97% of open abdominal surgeries. The most common complication of such adhesions is bowel obstruction, occurring in 15% of patients within 1 month of surgery. Our patient had an even more unique complication- constipation and dyssynergic defecation. Literature on post-op adhesions and defecation dysfunction mainly describes surgery of the rectal sphincter. In contrast, the sacrocolpopexy did not involve the rectum or surrounding peritoneum, but caused adhesions with a mass effect on the rectum. Given the morbidity associated with lower abdominal adhesions, suspicion must remain high in populations with a history of complicated abdominal surgery- especially for treatment of anterior pelvic floor disease.
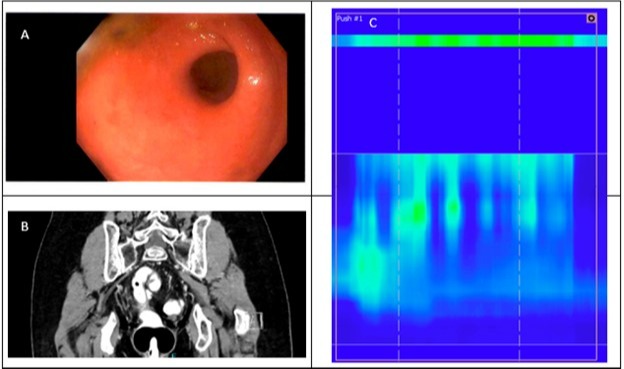
Figure: A. Flexible sigmoidoscopy: Very narrowed lumen in the sigmoid colon.
B. CT abdomen and pelvis: Coronal view showing sharp angulation in the sigmoid colon (due to the mass effect of the mesh and adhesions)
C.Anorectal manometry: The Y-axis notes length (cm) from anal sphincter (0cm) into sigmoid. The X-axis shows time (in seconds). The color of the data points denotes pressure exerted. Here, the top horizontal line in green shows rectal pressure. The same amount of pressure is shows in the bottom “green” areas, indicating that anal tone faily to appropriately relax. This increase in anal pressure with a good push, indicating dyssynergic defecation pattern.
B. CT abdomen and pelvis: Coronal view showing sharp angulation in the sigmoid colon (due to the mass effect of the mesh and adhesions)
C.Anorectal manometry: The Y-axis notes length (cm) from anal sphincter (0cm) into sigmoid. The X-axis shows time (in seconds). The color of the data points denotes pressure exerted. Here, the top horizontal line in green shows rectal pressure. The same amount of pressure is shows in the bottom “green” areas, indicating that anal tone faily to appropriately relax. This increase in anal pressure with a good push, indicating dyssynergic defecation pattern.
Disclosures:
David Lehoang indicated no relevant financial relationships.
Sean Dewberry indicated no relevant financial relationships.
Niharika Mallepally indicated no relevant financial relationships.
Christine Hsieh indicated no relevant financial relationships.
Sonia Sharma indicated no relevant financial relationships.
David Lehoang, MD, MBA, Sean Dewberry, , Niharika Mallepally, MD, MPH, Christine Hsieh, MD, Sonia Sharma, MD. B0276 - Stop, Drop, and Roll: One Woman’s Pelvic Floor Disease Journey, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
