Back

Poster Session D - Tuesday Morning
Category: Small Intestine
D0647 - A Case of Metastatic Melanoma of the Duodenum
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Naveen A. Mallangada, MD
Rutgers Robert Wood Johnson Medical School
New Brunswick, NJ
Presenting Author(s)
Eric Zhao, MD1, Naveen Mallangada, MD1, Kapil Gupta, MD2, Mahmoud A. Ali, MBBCh2, Anish Vinit Patel, MD2
1Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ; 2Rutgers Robert Wood Johnson University Hospital- New Brunswick, New Brunswick, NJ
Introduction: Malignant melanoma can metastasize to the small bowel. Symptoms are non-specific, and most patients go un-diagnosed during their lifetime. When found, surgical resection significantly improves survival; however, overall prognosis remains poor.
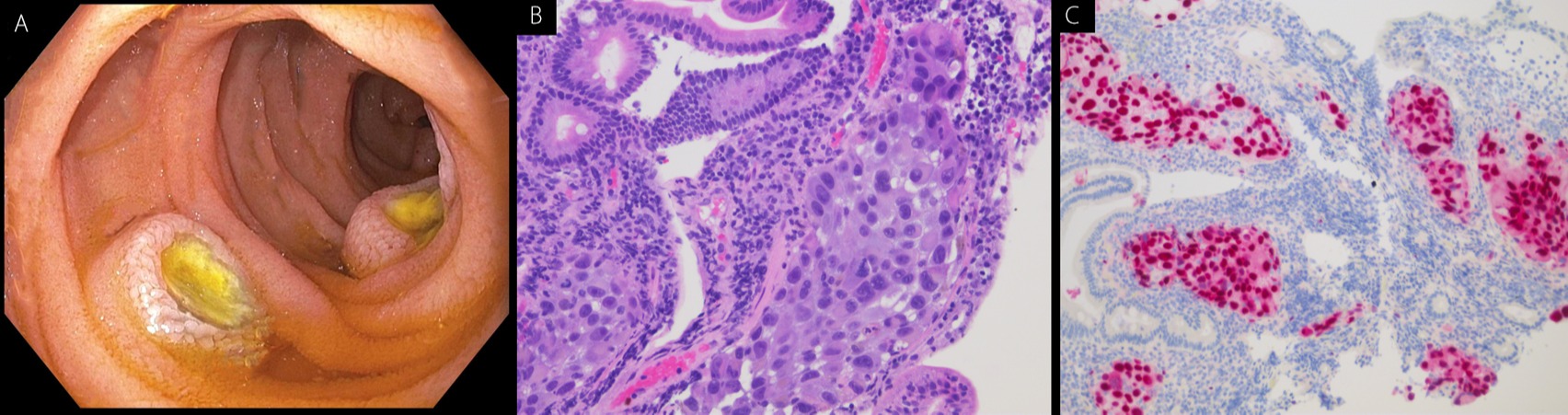
Case Description/Methods: A 63-year-old male with history of metastatic melanoma with metastasis to the lungs and brain presented with abdominal pain and intermittent hematochezia. He was previously diagnosed with immune mediated colitis related to ipilimumab and nivolumab therapy that had resolved with steroid therapy and infliximab. Computerized tomography (CT) of the abdomen-pelvis did not reveal any bowel abnormalities. Endoscopic evaluation was pursued. Colonoscopy did not reveal any mucosal disease. However, upper endoscopy revealed five large and small-sized ulcerated masses in the duodenum (Image A). Biopsies of these masses revealed metastatic melanoma (Image B) with positive SOX-10 immunostaining (Image C). The patient was started on new immunotherapy with plans for further management with oncology.
Discussion: We present here a case of metastatic melanoma of the duodenum. Melanoma is the fifth most common cancer in the United States. The small bowel is the most common site of gastrointestinal (GI) tract metastasis. However, most patients with metastatic intestinal melanoma go un-diagnosed, as only 1.5% to 4.4% receive a clinical diagnosis.
Common presentation of intestinal melanoma includes abdominal pain, anemia, obstruction and GI bleeding. Diagnostic modalities include abdominal ultrasound, contrast-enhanced CT, upper GI series, endoscopy, and capsule endoscopy. Imaging can reveal a polypoid mass with central ulceration, described as a target or a bulls-eye lesion. Endoscopic assessment typically reveals black colored ulcerated lesions. The treatment of choice for small bowel melanoma is complete resection. However, overall prognosis is still poor, as median survival for patients who undergo curative resection is 22 months. Immunotherapy is considered for multiple lesions.
In conclusion, patients with known melanoma presenting with GI symptoms should be evaluated for small bowel involvement, either radiologically or endoscopically. These patients should be approached with a high index of suspicion, as early detection and complete resection can significantly improve survival. Prior history of immune mediated enterocolitis should not preclude repeat thorough endoscopic evaluation when patients have new onset of GI symptoms.
Disclosures:
Eric Zhao, MD1, Naveen Mallangada, MD1, Kapil Gupta, MD2, Mahmoud A. Ali, MBBCh2, Anish Vinit Patel, MD2. D0647 - A Case of Metastatic Melanoma of the Duodenum, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ; 2Rutgers Robert Wood Johnson University Hospital- New Brunswick, New Brunswick, NJ
Introduction: Malignant melanoma can metastasize to the small bowel. Symptoms are non-specific, and most patients go un-diagnosed during their lifetime. When found, surgical resection significantly improves survival; however, overall prognosis remains poor.
Case Description/Methods: A 63-year-old male with history of metastatic melanoma with metastasis to the lungs and brain presented with abdominal pain and intermittent hematochezia. He was previously diagnosed with immune mediated colitis related to ipilimumab and nivolumab therapy that had resolved with steroid therapy and infliximab. Computerized tomography (CT) of the abdomen-pelvis did not reveal any bowel abnormalities. Endoscopic evaluation was pursued. Colonoscopy did not reveal any mucosal disease. However, upper endoscopy revealed five large and small-sized ulcerated masses in the duodenum (Image A). Biopsies of these masses revealed metastatic melanoma (Image B) with positive SOX-10 immunostaining (Image C). The patient was started on new immunotherapy with plans for further management with oncology.
Discussion: We present here a case of metastatic melanoma of the duodenum. Melanoma is the fifth most common cancer in the United States. The small bowel is the most common site of gastrointestinal (GI) tract metastasis. However, most patients with metastatic intestinal melanoma go un-diagnosed, as only 1.5% to 4.4% receive a clinical diagnosis.
Common presentation of intestinal melanoma includes abdominal pain, anemia, obstruction and GI bleeding. Diagnostic modalities include abdominal ultrasound, contrast-enhanced CT, upper GI series, endoscopy, and capsule endoscopy. Imaging can reveal a polypoid mass with central ulceration, described as a target or a bulls-eye lesion. Endoscopic assessment typically reveals black colored ulcerated lesions. The treatment of choice for small bowel melanoma is complete resection. However, overall prognosis is still poor, as median survival for patients who undergo curative resection is 22 months. Immunotherapy is considered for multiple lesions.
In conclusion, patients with known melanoma presenting with GI symptoms should be evaluated for small bowel involvement, either radiologically or endoscopically. These patients should be approached with a high index of suspicion, as early detection and complete resection can significantly improve survival. Prior history of immune mediated enterocolitis should not preclude repeat thorough endoscopic evaluation when patients have new onset of GI symptoms.
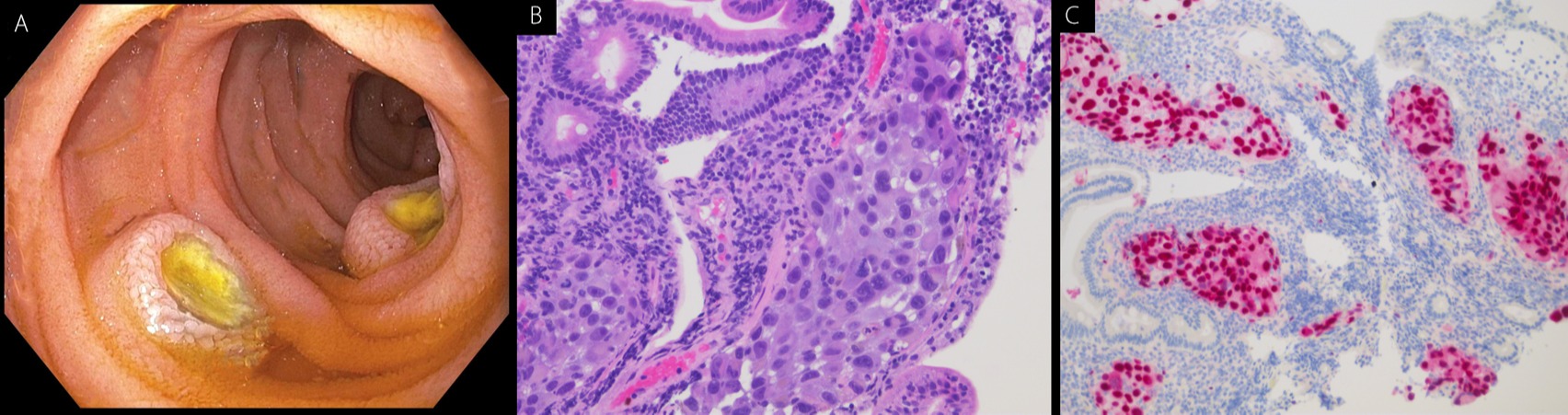
Figure: Image A: Endoscopic view of duodenal melanoma lesions
Image B, C: Histologic view of duodenal melanoma lesions
Image B, C: Histologic view of duodenal melanoma lesions
Disclosures:
Eric Zhao indicated no relevant financial relationships.
Naveen Mallangada indicated no relevant financial relationships.
Kapil Gupta indicated no relevant financial relationships.
Mahmoud Ali indicated no relevant financial relationships.
Anish Vinit Patel indicated no relevant financial relationships.
Eric Zhao, MD1, Naveen Mallangada, MD1, Kapil Gupta, MD2, Mahmoud A. Ali, MBBCh2, Anish Vinit Patel, MD2. D0647 - A Case of Metastatic Melanoma of the Duodenum, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
