Back

Poster Session D - Tuesday Morning
Category: Esophagus
D0238 - A Case of Idiopathic Hypereosinophilic Syndrome Involving the Gastrointestinal Tract
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- WC
Presenting Author(s)
Suhail Sidhu, BS1, Walter Crum, BS1, William S. Reiche, DO2, Thamer Kassim, MD1, Nicholas Dietz, MD1, Rajani Rangray, MBBS1
1Creighton University School of Medicine, Omaha, NE; 2CHI Creighton University Medical Center, Omaha, NE
Introduction: Hypereosinophilia (HE) is defined by an absolute eosinophil count greater than 1.5 k/mcL taken one month apart or by histologic confirmation of eosinophilic infiltration of the tissues. Hypereosinophilic syndrome (HES) occurs when HE causes organ damage. Complications from eosinophilic gastrointestinal (GI) disease include perforation, ischemic colitis, and portal vein thrombosis. Here we present a case of idiopathic HES involving multiple organs including the GI tract.
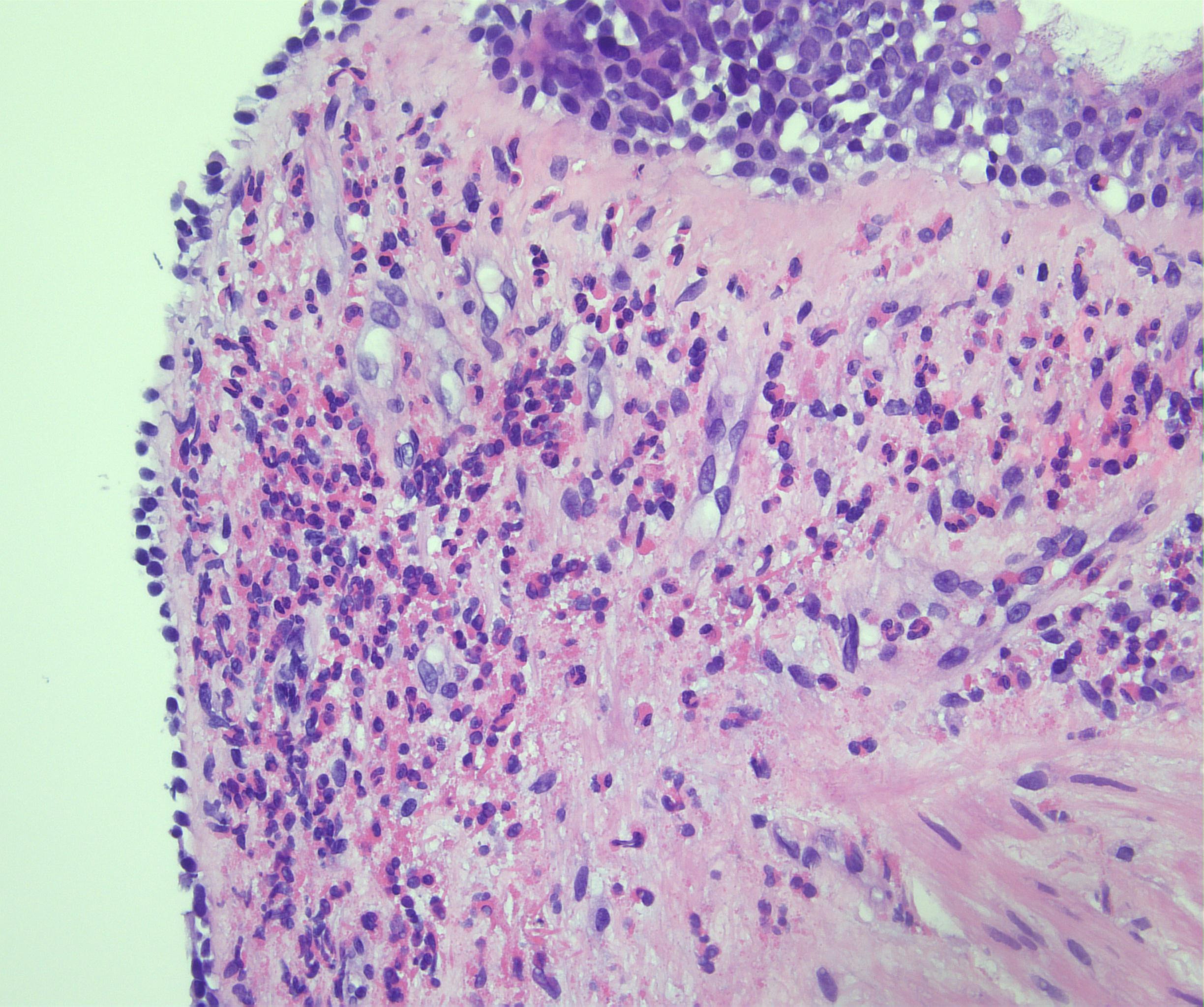
Case Description/Methods: A 39-year-old male presented to the hospital with three weeks of burning epigastric pain and diarrhea associated with fever; chills; fatigue; shortness of breath, and macular rash to the lower extremities. This began days after initiating a 12-day prednisone taper starting at 20 mg twice daily for presumed insect bite reaction. Eosinophils were 6.0 k/mcL on admission. Skin biopsy performed on lower extremities showed diffuse eosinophilic infiltration without evidence of vasculitis. Bronchoscopy revealed eosinophilic infiltration (92% eosinophils) without infection. ANA, anti-dsDNA, SSA, SSB, scleroderma antibody, C3, C4, RF, IgM, IgE, urine histoplasma antigen, serum coccidioides antibody, and antiphospholipid antibodies were within normal limits. With eosinophilic tissue infiltration associated with organ dysfunction and absolute eosinophil count >1.5 k/mcL, the patient met criteria for HES. Two doses of intravenous methylprednisolone 125 mg were administered before starting oral prednisone 60 mg AM and 20 mg PM for 90 days. The patient’s epigastric pain, shortness of breath, and pruritus resolved. Eosinophilia levels trended down from 9.3 k/mcL to 0.4 k/mcL within three days.
Discussion: While HES is primarily an immunological condition, it is important for physicians to be aware of eosinophilic manifestations of the GI tract. The patient’s severe epigastric pain and diarrhea were suggestive of eosinophilic gastroenteritis. He had skin and bronchial biopsies (Figure 1) along with peripheral eosinophilia and multiorgan involvement meeting criteria for idiopathic HES. Esophagogastroduodenoscopy and tissue sampling from the GI tract was not obtained as the patient responded well to treatment, hence adding an extra procedure wouldn't have altered the course of management. Early recognition of our patient’s symptoms led to a minimally invasive patient experience and a rapid response to therapy.
Disclosures:
Suhail Sidhu, BS1, Walter Crum, BS1, William S. Reiche, DO2, Thamer Kassim, MD1, Nicholas Dietz, MD1, Rajani Rangray, MBBS1. D0238 - A Case of Idiopathic Hypereosinophilic Syndrome Involving the Gastrointestinal Tract, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Creighton University School of Medicine, Omaha, NE; 2CHI Creighton University Medical Center, Omaha, NE
Introduction: Hypereosinophilia (HE) is defined by an absolute eosinophil count greater than 1.5 k/mcL taken one month apart or by histologic confirmation of eosinophilic infiltration of the tissues. Hypereosinophilic syndrome (HES) occurs when HE causes organ damage. Complications from eosinophilic gastrointestinal (GI) disease include perforation, ischemic colitis, and portal vein thrombosis. Here we present a case of idiopathic HES involving multiple organs including the GI tract.
Case Description/Methods: A 39-year-old male presented to the hospital with three weeks of burning epigastric pain and diarrhea associated with fever; chills; fatigue; shortness of breath, and macular rash to the lower extremities. This began days after initiating a 12-day prednisone taper starting at 20 mg twice daily for presumed insect bite reaction. Eosinophils were 6.0 k/mcL on admission. Skin biopsy performed on lower extremities showed diffuse eosinophilic infiltration without evidence of vasculitis. Bronchoscopy revealed eosinophilic infiltration (92% eosinophils) without infection. ANA, anti-dsDNA, SSA, SSB, scleroderma antibody, C3, C4, RF, IgM, IgE, urine histoplasma antigen, serum coccidioides antibody, and antiphospholipid antibodies were within normal limits. With eosinophilic tissue infiltration associated with organ dysfunction and absolute eosinophil count >1.5 k/mcL, the patient met criteria for HES. Two doses of intravenous methylprednisolone 125 mg were administered before starting oral prednisone 60 mg AM and 20 mg PM for 90 days. The patient’s epigastric pain, shortness of breath, and pruritus resolved. Eosinophilia levels trended down from 9.3 k/mcL to 0.4 k/mcL within three days.
Discussion: While HES is primarily an immunological condition, it is important for physicians to be aware of eosinophilic manifestations of the GI tract. The patient’s severe epigastric pain and diarrhea were suggestive of eosinophilic gastroenteritis. He had skin and bronchial biopsies (Figure 1) along with peripheral eosinophilia and multiorgan involvement meeting criteria for idiopathic HES. Esophagogastroduodenoscopy and tissue sampling from the GI tract was not obtained as the patient responded well to treatment, hence adding an extra procedure wouldn't have altered the course of management. Early recognition of our patient’s symptoms led to a minimally invasive patient experience and a rapid response to therapy.
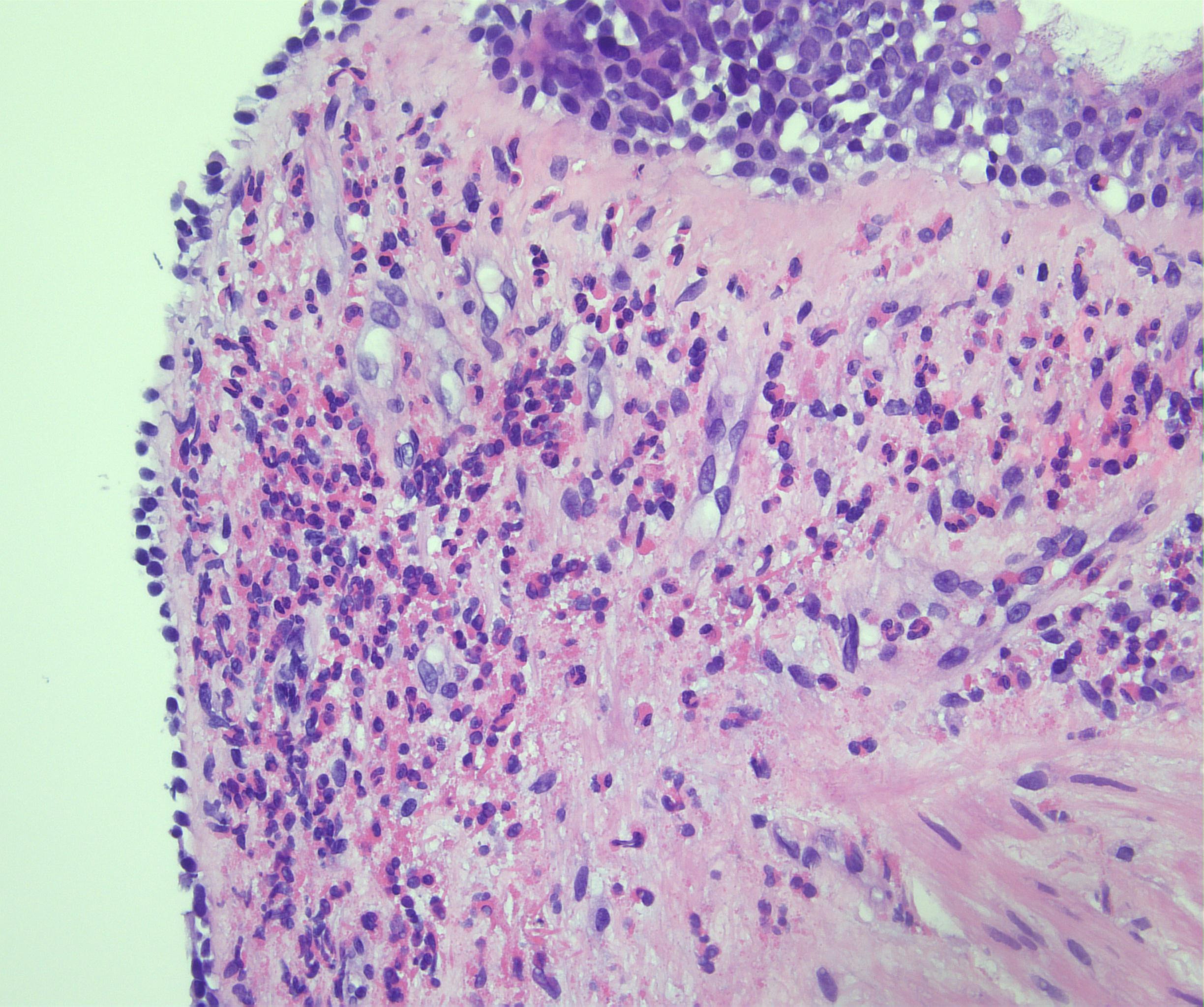
Figure: Biopsy of bronchial mucosa showing dense infiltration of eosinophils beneath the bronchial epithelium (greater than 50 per high power field). The granular pink cells are the eosinophils, largely on the left-hand side of the image (400X magnification, H&E stain).
Disclosures:
Suhail Sidhu indicated no relevant financial relationships.
Walter Crum indicated no relevant financial relationships.
William Reiche indicated no relevant financial relationships.
Thamer Kassim indicated no relevant financial relationships.
Nicholas Dietz indicated no relevant financial relationships.
Rajani Rangray indicated no relevant financial relationships.
Suhail Sidhu, BS1, Walter Crum, BS1, William S. Reiche, DO2, Thamer Kassim, MD1, Nicholas Dietz, MD1, Rajani Rangray, MBBS1. D0238 - A Case of Idiopathic Hypereosinophilic Syndrome Involving the Gastrointestinal Tract, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
