Back

Poster Session E - Tuesday Afternoon
Category: General Endoscopy
E0289 - Duodenal Hematoma With Partial SBO After Routine EGD in a Young Female Patient With No History of Hematologic Disorder
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Stefan Odabasic, MD
Trinity Health Livonia
Livonia, MI
Presenting Author(s)
Stefan Odabasic, MD1, Victoria Reick-Mitrisin, 2, Tushar Khanna, MD3, Zarak Hassan Khan, MD1, Nabil Sultani, MD1
1Trinity Health Livonia, Livonia, MI; 2A.T. Stills University, Livonia, MI; 3St. Mary Mercy Hospital, Livonia, MI
Introduction: Duodenal hematomas are a rare complication of endoscopic biopsy most often seen in children and young adults. Common factors include blunt trauma, anticoagulation, Henoch-Schonlein purpura and blood dyscrasias. They can cause significant morbidity and mortality, including duodenal obstruction, hospitalization and need for intravenous nutrition. Intramural hematomas are more commonly associated with complications. Treatment is generally conservative and consists of electrolyte replacement, decompression, and total parenteral nutrition. If conservative management fails, endoscopic or surgical interventions to relieve the hematoma are required.
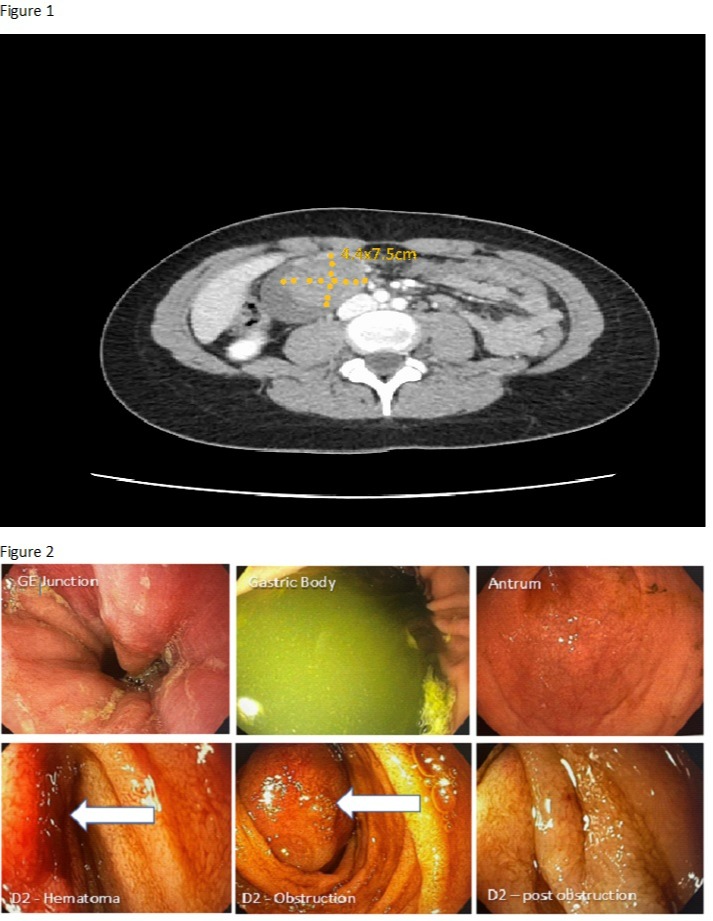
Case Description/Methods: A 22-year-old female with past medical history of chronic abdominal pain presented to the emergency department 7 hours after an uncomplicated esophagogastroduodenoscopy (EGD). She complained of abdominal pain, nausea, and vomiting. In the ED her vital signs were stable. Labs were remarkable for a mild leukocytosis and elevated total bilirubin. CT abdomen/pelvis was concerning for duodenal hematoma (Figure 1). Repeat EGD showed intramural duodenal hematoma at the biopsy site with no active bleeding (Figure 2). Patient was managed conservatively and discharged home with GI follow up. She returned to the ED at another hospital four days later for ongoing nausea, vomiting and abdominal pain. There was interval enlargement of the hematoma with increasing mass effect on the duodenum with no signs of infection or active bleeding. Consideration was given to endoscopic evacuation or percutaneous drainage. No invasive therapy was required, and she was discharged with GI follow up.
Discussion: Hemorrhages such as this one can lead to intramural accumulation of blood resulting in a hematoma that pulls fluid from the surrounding area by osmotic fluid shift. This forms an intraluminal bulge which can lead to duodenal occlusion causing compression on the pancreatic and biliary ducts. Typical symptoms include abdominal pain, nausea, and vomiting. Our patient was successfully managed conservatively. If conservative management fails, next step is endoscopic or surgical evacuation of the hematoma which is typically considered after 7-10 days of conservative therapy or if there are worsening complications. Newer therapies include ultrasonically guided drainage and balloon dilation. Our case illustrates the rare complication of intramural hematoma in a young adult, with no history of hematologic pathology, following routine EGD with duodenal biopsy.
Disclosures:
Stefan Odabasic, MD1, Victoria Reick-Mitrisin, 2, Tushar Khanna, MD3, Zarak Hassan Khan, MD1, Nabil Sultani, MD1. E0289 - Duodenal Hematoma With Partial SBO After Routine EGD in a Young Female Patient With No History of Hematologic Disorder, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Trinity Health Livonia, Livonia, MI; 2A.T. Stills University, Livonia, MI; 3St. Mary Mercy Hospital, Livonia, MI
Introduction: Duodenal hematomas are a rare complication of endoscopic biopsy most often seen in children and young adults. Common factors include blunt trauma, anticoagulation, Henoch-Schonlein purpura and blood dyscrasias. They can cause significant morbidity and mortality, including duodenal obstruction, hospitalization and need for intravenous nutrition. Intramural hematomas are more commonly associated with complications. Treatment is generally conservative and consists of electrolyte replacement, decompression, and total parenteral nutrition. If conservative management fails, endoscopic or surgical interventions to relieve the hematoma are required.
Case Description/Methods: A 22-year-old female with past medical history of chronic abdominal pain presented to the emergency department 7 hours after an uncomplicated esophagogastroduodenoscopy (EGD). She complained of abdominal pain, nausea, and vomiting. In the ED her vital signs were stable. Labs were remarkable for a mild leukocytosis and elevated total bilirubin. CT abdomen/pelvis was concerning for duodenal hematoma (Figure 1). Repeat EGD showed intramural duodenal hematoma at the biopsy site with no active bleeding (Figure 2). Patient was managed conservatively and discharged home with GI follow up. She returned to the ED at another hospital four days later for ongoing nausea, vomiting and abdominal pain. There was interval enlargement of the hematoma with increasing mass effect on the duodenum with no signs of infection or active bleeding. Consideration was given to endoscopic evacuation or percutaneous drainage. No invasive therapy was required, and she was discharged with GI follow up.
Discussion: Hemorrhages such as this one can lead to intramural accumulation of blood resulting in a hematoma that pulls fluid from the surrounding area by osmotic fluid shift. This forms an intraluminal bulge which can lead to duodenal occlusion causing compression on the pancreatic and biliary ducts. Typical symptoms include abdominal pain, nausea, and vomiting. Our patient was successfully managed conservatively. If conservative management fails, next step is endoscopic or surgical evacuation of the hematoma which is typically considered after 7-10 days of conservative therapy or if there are worsening complications. Newer therapies include ultrasonically guided drainage and balloon dilation. Our case illustrates the rare complication of intramural hematoma in a young adult, with no history of hematologic pathology, following routine EGD with duodenal biopsy.
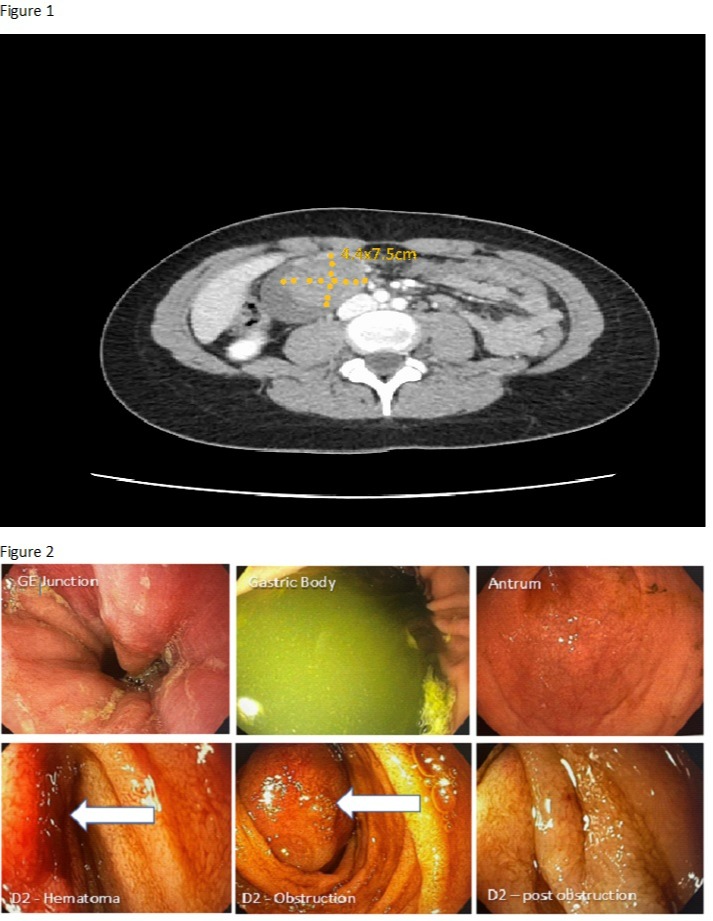
Figure: Figure 1 - CT abdomen/pelvis showing duodenal hematoma
Figure 2 - EGD images showing GE junction, gastric contents, antrum, intramural hematoma in the 2nd portion of the duodenum and 2nd portion of duodenum distal to obstruction
Figure 2 - EGD images showing GE junction, gastric contents, antrum, intramural hematoma in the 2nd portion of the duodenum and 2nd portion of duodenum distal to obstruction
Disclosures:
Stefan Odabasic indicated no relevant financial relationships.
Victoria Reick-Mitrisin indicated no relevant financial relationships.
Tushar Khanna indicated no relevant financial relationships.
Zarak Hassan Khan indicated no relevant financial relationships.
Nabil Sultani indicated no relevant financial relationships.
Stefan Odabasic, MD1, Victoria Reick-Mitrisin, 2, Tushar Khanna, MD3, Zarak Hassan Khan, MD1, Nabil Sultani, MD1. E0289 - Duodenal Hematoma With Partial SBO After Routine EGD in a Young Female Patient With No History of Hematologic Disorder, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
