Back


Poster Session E - Tuesday Afternoon
Category: General Endoscopy
E0290 - A Rare Case of Erosive Gastritis and Melena Related to Gastric Mucosal Calcinosis
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Has Audio
Patrick J. Carey, MD
University of Kentucky College of Medcine, KY
Presenting Author(s)
Patrick J. Carey, MD, Kyle Fischer, MD, Ahmed Al-Chalabi, MD
University of Kentucky College of Medcine, Lexington, KY
Introduction: Gastric mucosal calcinosis (GMC) is a rare disorder typically found incidentally or at autopsy. GMC can rarely lead to upper gastrointestinal bleeding if it results in severe erosive or ulcerative gastritis. We present a case of a patient with GMC secondary to End-Stage Renal Disease (ESRD).
Case Description/Methods: A 74-year-old male with history of ESRD on peritoneal dialysis, atrial fibrillation, HFrEF, and hypothyroidism was admitted for generalized weakness, abdominal pain, and four days of melena. He had been hospitalized one week prior for peritonitis, which was treated with vancomycin and ceftazidime. Review of systems was also notable for odynophagia. He denied dyspnea, chest pain, hematochezia, or hematemesis. Vital signs were notable for tachycardia but were otherwise within normal limits. Physical exam was significant for an irregularly irregular cardiac rhythm, mild abdominal distension, and moderate diffuse abdominal tenderness. Labs were notable for white cell count of 16 per µl, hemoglobin 7.7 g/dl, platelets 236,000 per µl, K 2.5 mmol/l, Ca 6.4 mmol/l, and phosphorus 4.2 mmol/l. CT images showed mild wall thickening of the descending and sigmoid colon with mild mesenteric stranding which may represent colitis. Stool PCR was positive for Clostridium difficile.
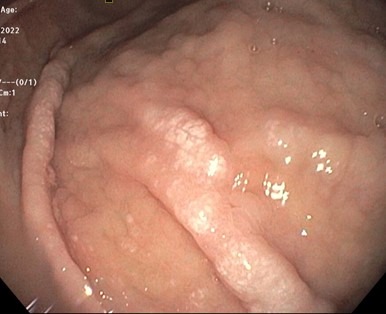
He subsequently underwent esophagogastroduodenoscopy (EGD) that demonstrated patchy areas of whitish mucosa (Figure 1) associated with moderate gastric erythema, edema, and erosions in addition to thickening of gastric folds. Gastric biopsies revealed gastric mucosal calcinosis. He was started on fidaxomicin for C. diff colitis. He was continued on proton pump inhibitors with resolution of his melena.
Discussion: GMC, as found in this patient, can be part of metastatic calcinosis, which is the most common type of GMC. It can occur in up to 13% of ESRD patients. Gastric tissue is thought to be more prone to calcification given its relatively intracellular alkalinity. Endoscopic evidence of gastric calcifications is generally seen as 1-5mm white flat plaques in fundus, body, or antrum. Diagnosis is important in this patient population as GMC can rarely cause ulcerations/necrosis of gastric tissue leading to acute upper gastrointestinal bleeding. Therefore, GMC should be always considered in the differential diagnosis in patients with long history of ESRD presenting with melena.
Disclosures:
Patrick J. Carey, MD, Kyle Fischer, MD, Ahmed Al-Chalabi, MD. E0290 - A Rare Case of Erosive Gastritis and Melena Related to Gastric Mucosal Calcinosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
University of Kentucky College of Medcine, Lexington, KY
Introduction: Gastric mucosal calcinosis (GMC) is a rare disorder typically found incidentally or at autopsy. GMC can rarely lead to upper gastrointestinal bleeding if it results in severe erosive or ulcerative gastritis. We present a case of a patient with GMC secondary to End-Stage Renal Disease (ESRD).
Case Description/Methods: A 74-year-old male with history of ESRD on peritoneal dialysis, atrial fibrillation, HFrEF, and hypothyroidism was admitted for generalized weakness, abdominal pain, and four days of melena. He had been hospitalized one week prior for peritonitis, which was treated with vancomycin and ceftazidime. Review of systems was also notable for odynophagia. He denied dyspnea, chest pain, hematochezia, or hematemesis. Vital signs were notable for tachycardia but were otherwise within normal limits. Physical exam was significant for an irregularly irregular cardiac rhythm, mild abdominal distension, and moderate diffuse abdominal tenderness. Labs were notable for white cell count of 16 per µl, hemoglobin 7.7 g/dl, platelets 236,000 per µl, K 2.5 mmol/l, Ca 6.4 mmol/l, and phosphorus 4.2 mmol/l. CT images showed mild wall thickening of the descending and sigmoid colon with mild mesenteric stranding which may represent colitis. Stool PCR was positive for Clostridium difficile.
He subsequently underwent esophagogastroduodenoscopy (EGD) that demonstrated patchy areas of whitish mucosa (Figure 1) associated with moderate gastric erythema, edema, and erosions in addition to thickening of gastric folds. Gastric biopsies revealed gastric mucosal calcinosis. He was started on fidaxomicin for C. diff colitis. He was continued on proton pump inhibitors with resolution of his melena.
Discussion: GMC, as found in this patient, can be part of metastatic calcinosis, which is the most common type of GMC. It can occur in up to 13% of ESRD patients. Gastric tissue is thought to be more prone to calcification given its relatively intracellular alkalinity. Endoscopic evidence of gastric calcifications is generally seen as 1-5mm white flat plaques in fundus, body, or antrum. Diagnosis is important in this patient population as GMC can rarely cause ulcerations/necrosis of gastric tissue leading to acute upper gastrointestinal bleeding. Therefore, GMC should be always considered in the differential diagnosis in patients with long history of ESRD presenting with melena.
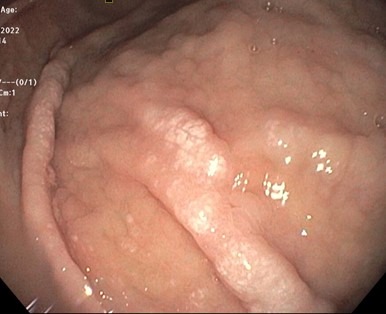
Figure: Figure 1. Endoscopic appearance of gastric mucosal calcinosis
Disclosures:
Patrick Carey indicated no relevant financial relationships.
Kyle Fischer indicated no relevant financial relationships.
Ahmed Al-Chalabi indicated no relevant financial relationships.
Patrick J. Carey, MD, Kyle Fischer, MD, Ahmed Al-Chalabi, MD. E0290 - A Rare Case of Erosive Gastritis and Melena Related to Gastric Mucosal Calcinosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
