Back

Poster Session E - Tuesday Afternoon
Category: General Endoscopy
E0291 - Threading the Needle: Safely Removing Double-Edged Sharp Foreign Bodies
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Andrew Krane, MD
Warren Alpert Medical School of Brown University
Providence, RI
Presenting Author(s)
Andrew Krane, MD1, George M. Hanna, MD1, Kanhai Farrakhan, MD2, Thomas E. Sepe, MD, FACG3
1Warren Alpert Medical School of Brown University, Providence, RI; 2Lifespan, Providence, RI; 3University Gastroenterology, Providence, RI
Introduction: Foreign body ingestion is a common phenomenon among individuals with psychiatric disorders, alcohol intoxication, developmental delay, or in incarcerated individuals. Most ingested foreign bodies pass spontaneously without complication but 10-20% require endoscopic intervention. Impaction, perforation, or obstruction often occurs at angulations or narrowing. Early recognition and urgent upper endoscopy (EGD) for foreign body removal may improve clinical outcomes. Here we present a case of melena and abdominal pain secondary to foreign body ingestion.
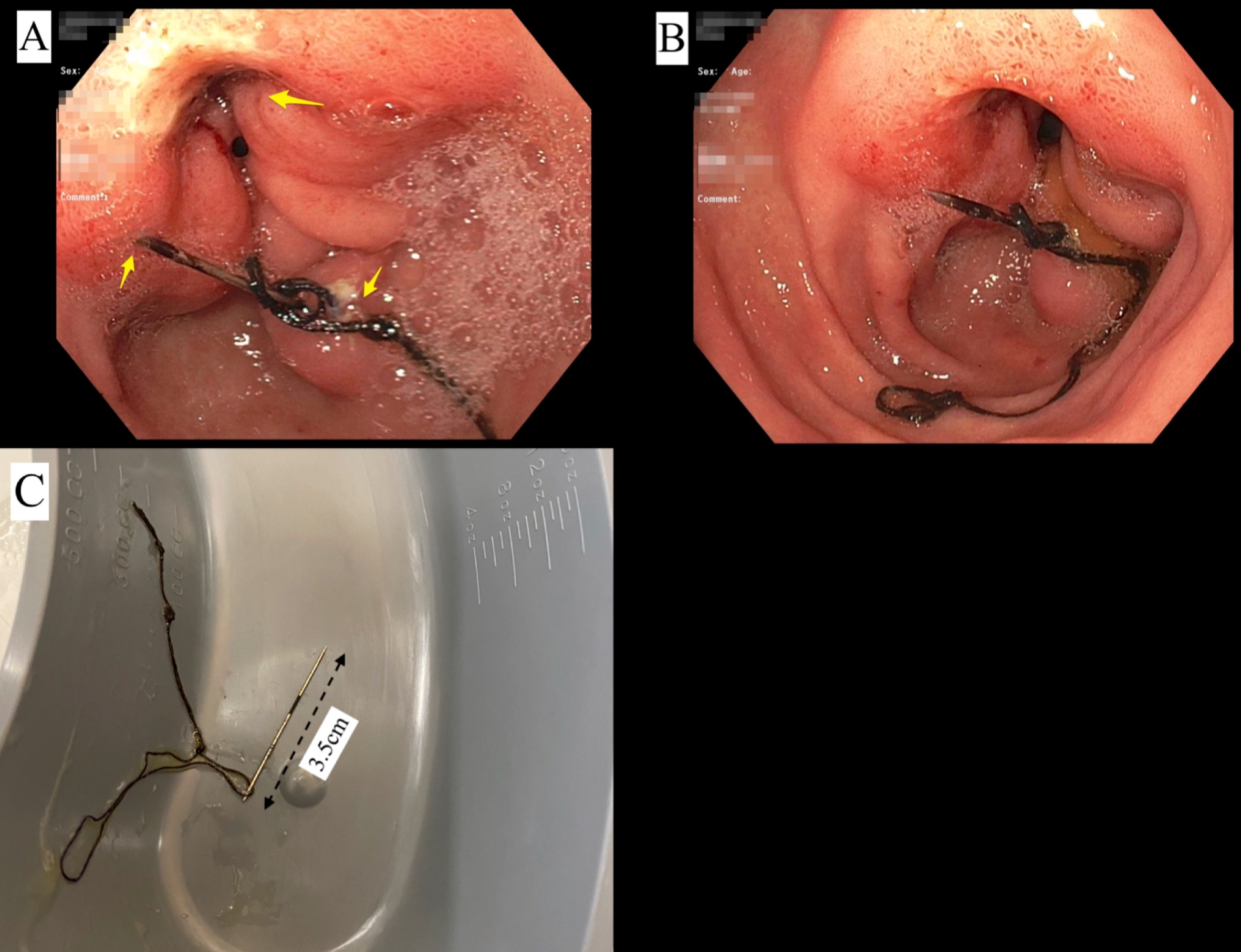
Case Description/Methods: An 83-year-old male with a past medical history of pulmonary embolism on warfarin, alcohol use disorder, and anxiety presented after two black, tarry stools and light-headedness. On admission his vitals were stable and labs were notable for an International normalized ratio (INR) of 3.3 and a Hemoglobin (Hgb) of 12.3g/dL. He was treated with Vitamin K and intravenous pantoprazole twice daily. The next day his Hgb was found to be 8.2g/dL and an EGD was performed revealing antral ulcerations and a 3.5cm sewing needle and thread with both ends penetrating opposite walls of the antrum (Figure A, B). Multiple attempts at removing the needle with rat tooth and jumbo forceps were unsuccessful and the procedure was aborted. Follow up computed tomography imaging did not reveal perigastric fluid or pneumoperitoneum post-procedurally. On hospital day three a repeat EGD was attempted and showed the needle was only perforating mucosa along one side of the gastric body; it was able to be removed via overtube and raptor device (Figure C).
Discussion: Endoscopic removal of sharp ingested foreign bodies can prove to be challenging. Several risk factors including age and duration of impaction are associated with adverse events, such as laceration, perforation, and ulcers. Double pointed/sharp objects are particularly challenging given they are harder to grasp and maneuver. That, in addition to luminal contractions, likely contributed to the difficulty retrieving the needle in this case despite using recommended tools. Had the second endoscopic retrieval attempt failed, the patient would have required surgical evaluation. Overall, the benefit of further endoscopic retrieval attempts versus the risk of perforation from the foreign body or complications from the procedure itself must be weighed case by case.
Disclosures:
Andrew Krane, MD1, George M. Hanna, MD1, Kanhai Farrakhan, MD2, Thomas E. Sepe, MD, FACG3. E0291 - Threading the Needle: Safely Removing Double-Edged Sharp Foreign Bodies, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Warren Alpert Medical School of Brown University, Providence, RI; 2Lifespan, Providence, RI; 3University Gastroenterology, Providence, RI
Introduction: Foreign body ingestion is a common phenomenon among individuals with psychiatric disorders, alcohol intoxication, developmental delay, or in incarcerated individuals. Most ingested foreign bodies pass spontaneously without complication but 10-20% require endoscopic intervention. Impaction, perforation, or obstruction often occurs at angulations or narrowing. Early recognition and urgent upper endoscopy (EGD) for foreign body removal may improve clinical outcomes. Here we present a case of melena and abdominal pain secondary to foreign body ingestion.
Case Description/Methods: An 83-year-old male with a past medical history of pulmonary embolism on warfarin, alcohol use disorder, and anxiety presented after two black, tarry stools and light-headedness. On admission his vitals were stable and labs were notable for an International normalized ratio (INR) of 3.3 and a Hemoglobin (Hgb) of 12.3g/dL. He was treated with Vitamin K and intravenous pantoprazole twice daily. The next day his Hgb was found to be 8.2g/dL and an EGD was performed revealing antral ulcerations and a 3.5cm sewing needle and thread with both ends penetrating opposite walls of the antrum (Figure A, B). Multiple attempts at removing the needle with rat tooth and jumbo forceps were unsuccessful and the procedure was aborted. Follow up computed tomography imaging did not reveal perigastric fluid or pneumoperitoneum post-procedurally. On hospital day three a repeat EGD was attempted and showed the needle was only perforating mucosa along one side of the gastric body; it was able to be removed via overtube and raptor device (Figure C).
Discussion: Endoscopic removal of sharp ingested foreign bodies can prove to be challenging. Several risk factors including age and duration of impaction are associated with adverse events, such as laceration, perforation, and ulcers. Double pointed/sharp objects are particularly challenging given they are harder to grasp and maneuver. That, in addition to luminal contractions, likely contributed to the difficulty retrieving the needle in this case despite using recommended tools. Had the second endoscopic retrieval attempt failed, the patient would have required surgical evaluation. Overall, the benefit of further endoscopic retrieval attempts versus the risk of perforation from the foreign body or complications from the procedure itself must be weighed case by case.
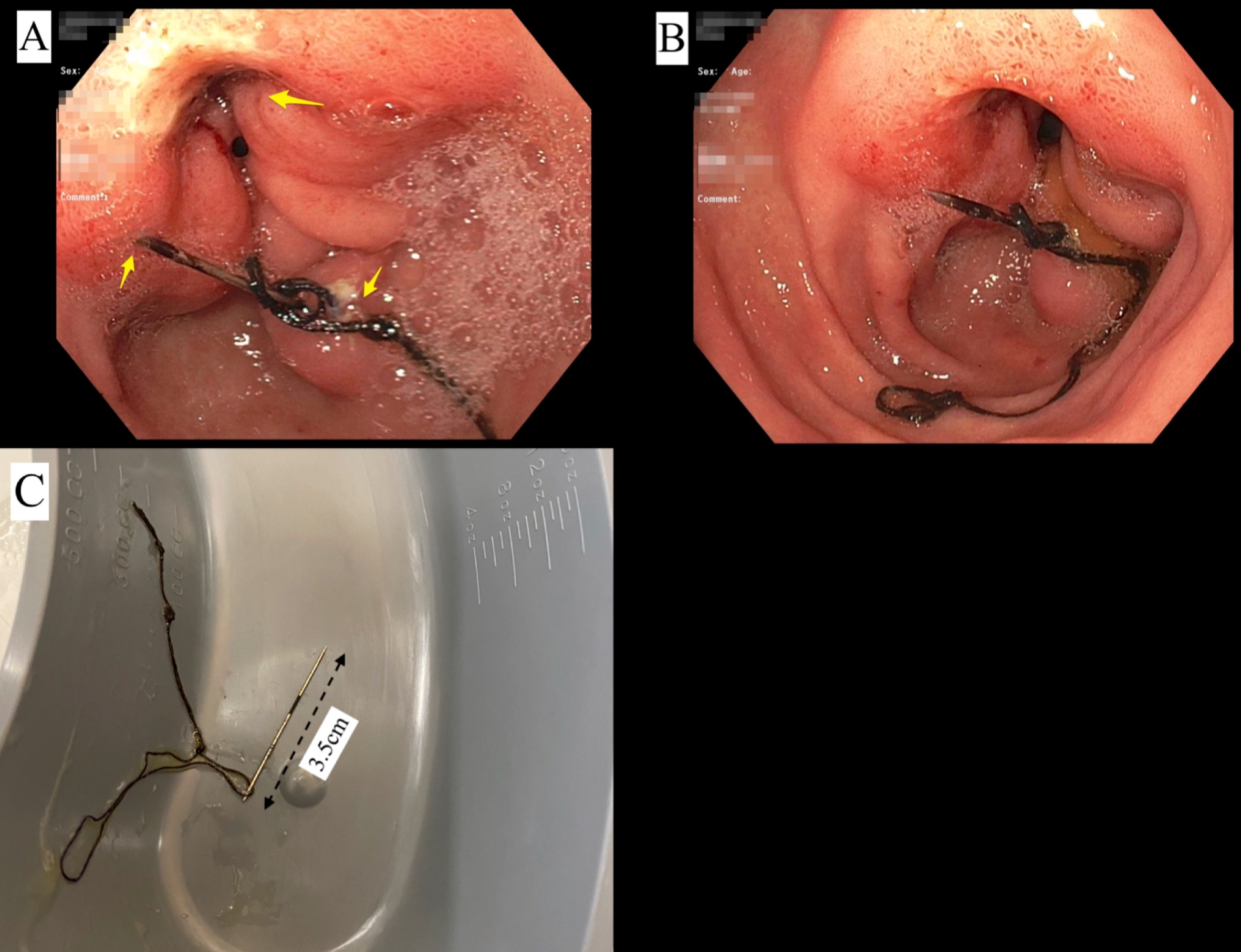
Figure: Figure 1: Endoscopic Evaluation of Patient with Foreign Body
A – Foreign body wedged between opposite ends of pylorus (Highlighted by top arrow)
B – Full view of sewing needle with thread in gastric antrum
C – Sewing needle after removal
A – Foreign body wedged between opposite ends of pylorus (Highlighted by top arrow)
B – Full view of sewing needle with thread in gastric antrum
C – Sewing needle after removal
Disclosures:
Andrew Krane indicated no relevant financial relationships.
George Hanna indicated no relevant financial relationships.
Kanhai Farrakhan indicated no relevant financial relationships.
Thomas Sepe indicated no relevant financial relationships.
Andrew Krane, MD1, George M. Hanna, MD1, Kanhai Farrakhan, MD2, Thomas E. Sepe, MD, FACG3. E0291 - Threading the Needle: Safely Removing Double-Edged Sharp Foreign Bodies, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
