Back

Poster Session B - Monday Morning
Category: Colon
B0124 - An Unusual Case of Diarrhea in an Immunosuppressed Patient
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Deepa P. Budh, MD
St. Barnabas Health System
Bronx, NY
Presenting Author(s)
Deepa P. Budh, MD1, Dushyant Dahiya, MD2, Rajat Garg, MD3, Amandeep Singh, MD4
1St. Barnabas Health System, Bronx, NY; 2Central Michigan University, Mount Pleasant, MI; 3Cleveland Clinic Foundation, Cleveland, OH; 4Cleveland Clinic Foundation, Beachwood, OH
Introduction: Amoebic Colitis, a frequent clinical manifestation of invasive intestinal infection due to Entamoeba histolytica, is a common cause of diarrhea mostly prevalent in developing countries due to unsanitary conditions. Although 90% of the cases may be asymptomatic carriers, one of the most common clinical manifestations include dysentery. It carries an excellent prognosis if diagnosed promptly and treated. However, establishing a diagnosis of Amoebic Colitis is often challenging. We highlight a unique case of Amoebic Colitis in a 73-year-old female in a setting of immunosuppression.
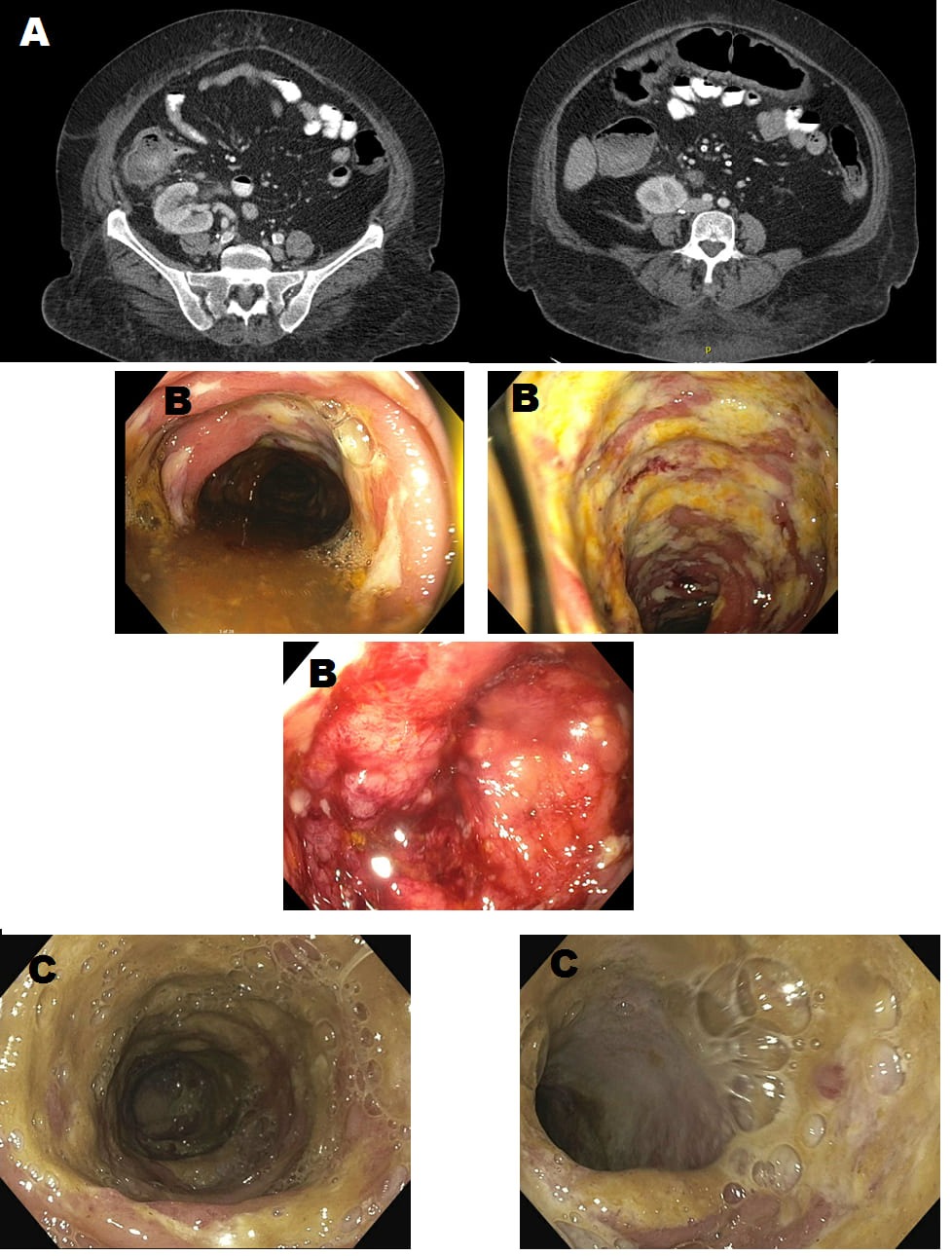
Case Description/Methods: A 73-year-old female from Qatar with ESRD, DM, HTN, and Renal cell carcinoma was admitted for abdominal pain, bloody diarrhea, and on and off a fever for 3 months. She was on tacrolimus, mycophenolate, and prednisone for her renal transplant. Diffuse abdominal tenderness was noted on examination but vitals were normal. CT scan showed ascending and transverse colon colitis and colonoscopy showed congested rectal, rectosigmoid, and sigmoid colon mucosa with multiple ulcers in descending, transverse, and ascending colon and rectum. Stool calprotectin was >3000 mg/kg Biopsy results showed active colitis with ulcers. Intravenous steroids were started and she showed improvement but abdominal pain and bloody diarrhea recurred with rise in CRP (from 6.9 to 15.5 mg/kg) when she was switched to oral steroids. A repeat CT scan showed an increase in the involvement of the right colon and piperacillin-tazobactam was started. Repeat colonoscopy showed a vascular pattern in mucosa diffusely decreased and nonbleeding ulcerated mucosa. Meanwhile, the E. histolytica antibody was positive. Antibiotics were switched to oral metronidazole. Pathology showed chronic active colitis with ulcer and increase apoptotic crypt epithelial cells. The clinical condition continued to improve and she was discharged home on steroid taper with a plan to repeat the scope in 3 months. She is doing well and on regular follow-up.
Discussion: Amoebic colitis should be a differential diagnosis for individuals from eastern countries where the prevalence of Entamoeba histolytica continues to be high as a delay in diagnosis may lead to adverse outcomes. Diagnosis often requires a combination of different modalities including stool microscopy, stool antigen testing, and colonic biopsies. Treatment with metronidazole, tinidazole, paromomycin, diiodohydroxyquin, or diloxanide furoate is often highly safe and effective.
Disclosures:
Deepa P. Budh, MD1, Dushyant Dahiya, MD2, Rajat Garg, MD3, Amandeep Singh, MD4. B0124 - An Unusual Case of Diarrhea in an Immunosuppressed Patient, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1St. Barnabas Health System, Bronx, NY; 2Central Michigan University, Mount Pleasant, MI; 3Cleveland Clinic Foundation, Cleveland, OH; 4Cleveland Clinic Foundation, Beachwood, OH
Introduction: Amoebic Colitis, a frequent clinical manifestation of invasive intestinal infection due to Entamoeba histolytica, is a common cause of diarrhea mostly prevalent in developing countries due to unsanitary conditions. Although 90% of the cases may be asymptomatic carriers, one of the most common clinical manifestations include dysentery. It carries an excellent prognosis if diagnosed promptly and treated. However, establishing a diagnosis of Amoebic Colitis is often challenging. We highlight a unique case of Amoebic Colitis in a 73-year-old female in a setting of immunosuppression.
Case Description/Methods: A 73-year-old female from Qatar with ESRD, DM, HTN, and Renal cell carcinoma was admitted for abdominal pain, bloody diarrhea, and on and off a fever for 3 months. She was on tacrolimus, mycophenolate, and prednisone for her renal transplant. Diffuse abdominal tenderness was noted on examination but vitals were normal. CT scan showed ascending and transverse colon colitis and colonoscopy showed congested rectal, rectosigmoid, and sigmoid colon mucosa with multiple ulcers in descending, transverse, and ascending colon and rectum. Stool calprotectin was >3000 mg/kg Biopsy results showed active colitis with ulcers. Intravenous steroids were started and she showed improvement but abdominal pain and bloody diarrhea recurred with rise in CRP (from 6.9 to 15.5 mg/kg) when she was switched to oral steroids. A repeat CT scan showed an increase in the involvement of the right colon and piperacillin-tazobactam was started. Repeat colonoscopy showed a vascular pattern in mucosa diffusely decreased and nonbleeding ulcerated mucosa. Meanwhile, the E. histolytica antibody was positive. Antibiotics were switched to oral metronidazole. Pathology showed chronic active colitis with ulcer and increase apoptotic crypt epithelial cells. The clinical condition continued to improve and she was discharged home on steroid taper with a plan to repeat the scope in 3 months. She is doing well and on regular follow-up.
Discussion: Amoebic colitis should be a differential diagnosis for individuals from eastern countries where the prevalence of Entamoeba histolytica continues to be high as a delay in diagnosis may lead to adverse outcomes. Diagnosis often requires a combination of different modalities including stool microscopy, stool antigen testing, and colonic biopsies. Treatment with metronidazole, tinidazole, paromomycin, diiodohydroxyquin, or diloxanide furoate is often highly safe and effective.
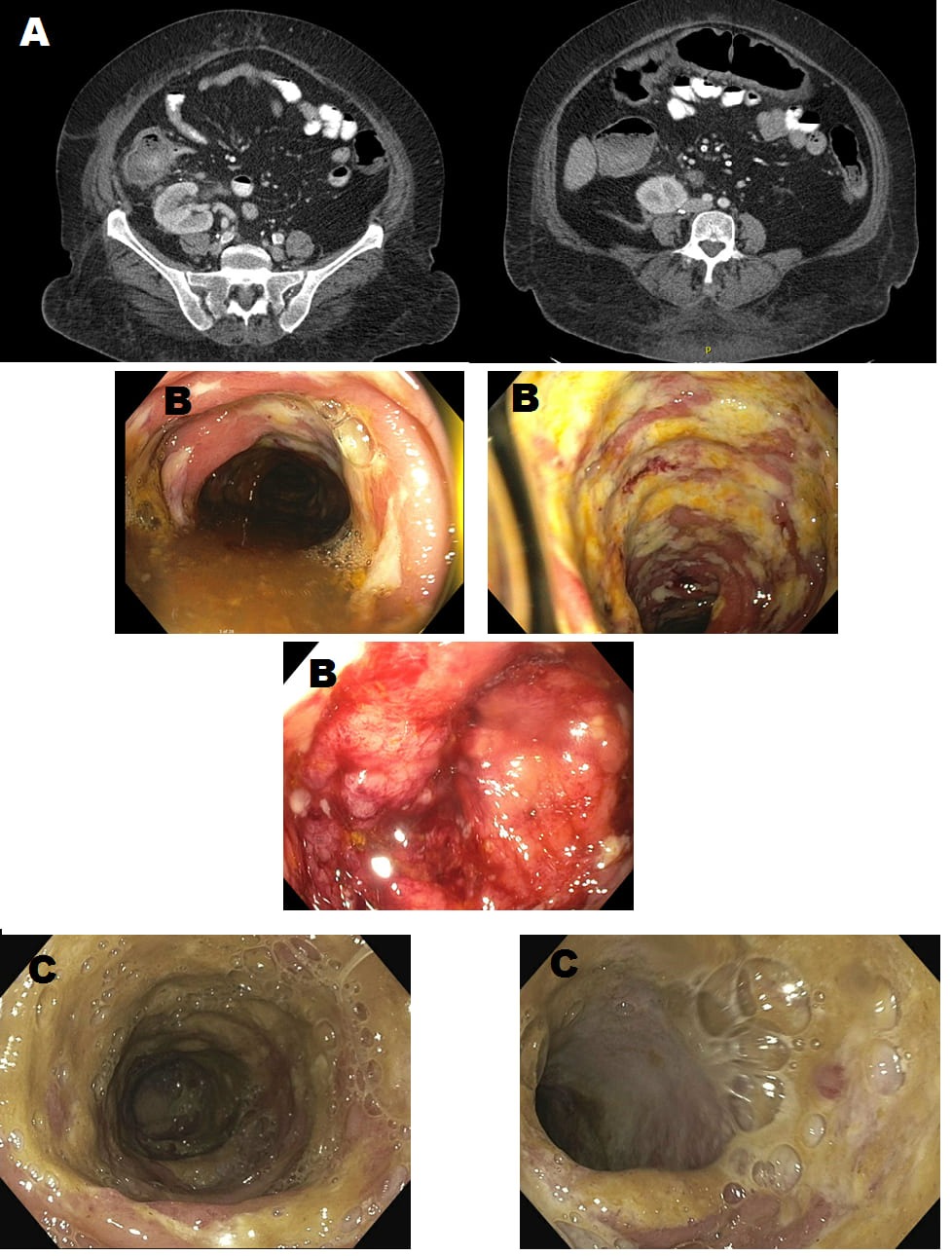
Figure: Image1 :
A- Ascending and transverse colonic wall thickening consistent with colitis
B - Congested, friable, and ulcerated mucosa
C- The mucosa vascular pattern in the descending colon was diffusely decreased- after treatment
A- Ascending and transverse colonic wall thickening consistent with colitis
B - Congested, friable, and ulcerated mucosa
C- The mucosa vascular pattern in the descending colon was diffusely decreased- after treatment
Disclosures:
Deepa Budh indicated no relevant financial relationships.
Dushyant Dahiya indicated no relevant financial relationships.
Rajat Garg indicated no relevant financial relationships.
Amandeep Singh indicated no relevant financial relationships.
Deepa P. Budh, MD1, Dushyant Dahiya, MD2, Rajat Garg, MD3, Amandeep Singh, MD4. B0124 - An Unusual Case of Diarrhea in an Immunosuppressed Patient, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
