Back

Poster Session C - Monday Afternoon
Category: Colon
C0163 - Chronic Antibiotic-Resistant Pouchitis: A Complicated Entity
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Aditya Chauhan, MD
The Brooklyn Hospital Center
Brooklyn, NY
Presenting Author(s)
Aditya Chauhan, MD1, Vijay Gayam, MD1, Praneeth Bandaru, MD1, Srilaxmi Gujjula, MD1, Erika Vigandt, MD1, Vikash Kumar, MD1, Denzil Etienne, MD1, Kimberly Geckle, APRN-CNP2, Heidi Budke, MD2, Vinaya Gaduputi, MD, FACG2
1The Brooklyn Hospital Center, Brooklyn, NY; 2Blanchard Valley Health System, Findlay, OH
Introduction: Patients who undergo restorative proctocolectomy and ileoanal anastomosis can develop pouchitis as a common chronic complication. A rare subset of patients fails to respond to multiple antibiotic therapies and develop chronic antibiotic refractory pouchitis (CARP). We present a case of a 45-year-old male with pouchitis refractory to chronic antibiotic therapy and histology demonstrating chronic inflammatory changes.
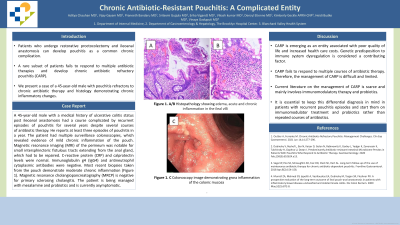
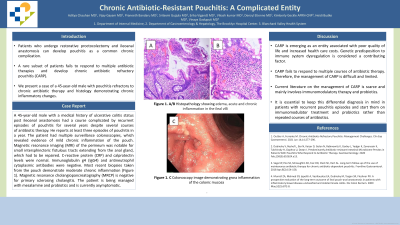
Case Description/Methods: A 45-year-old male with a medical history of ulcerative colitis status post ileoanal anastomosis had a course complicated by recurrent episodes of pouchitis for several years despite several courses of antibiotic therapy. He reports at least three episodes of pouchitis in a year. The patient had multiple surveillance colonoscopies, which revealed evidence of mild chronic inflammation of the pouch. Magnetic resonance imaging (MRI) of the perineum was notable for small intersphincteric fistulous tracts extending from the anal gland, which had to be repaired. C-reactive protein (CRP) and calprotectin levels were normal. Immunoglobulin g4 (IgG4) and antineutrophil cytoplasmic antibodies were negative. Most recent biopsies taken from the pouch demonstrate moderate chronic inflammation (figure 1). Magnetic resonance cholangiopancreatography (MRCP) is negative for primary sclerosing cholangitis. The patient is being managed with mesalamine and probiotics and is currently asymptomatic.
Discussion: CARP is emerging as an entity associated with poor quality of life and increased health care costs. Genetic predisposition to immune system dysregulation is considered a contributing factor. CARP fails to respond to multiple courses of antibiotic therapy. Therefore, the management of CARP is difficult and limited. Current literature on the management of CARP is scarce and mainly involves immunomodulatory therapy and probiotics. It is essential to keep this differential diagnosis in mind in patients with recurrent pouchitis episodes and start them on immunomodulator treatment and probiotics rather than repeated courses of antibiotics.

Disclosures:
Aditya Chauhan, MD1, Vijay Gayam, MD1, Praneeth Bandaru, MD1, Srilaxmi Gujjula, MD1, Erika Vigandt, MD1, Vikash Kumar, MD1, Denzil Etienne, MD1, Kimberly Geckle, APRN-CNP2, Heidi Budke, MD2, Vinaya Gaduputi, MD, FACG2. C0163 - Chronic Antibiotic-Resistant Pouchitis: A Complicated Entity, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1The Brooklyn Hospital Center, Brooklyn, NY; 2Blanchard Valley Health System, Findlay, OH
Introduction: Patients who undergo restorative proctocolectomy and ileoanal anastomosis can develop pouchitis as a common chronic complication. A rare subset of patients fails to respond to multiple antibiotic therapies and develop chronic antibiotic refractory pouchitis (CARP). We present a case of a 45-year-old male with pouchitis refractory to chronic antibiotic therapy and histology demonstrating chronic inflammatory changes.
Case Description/Methods: A 45-year-old male with a medical history of ulcerative colitis status post ileoanal anastomosis had a course complicated by recurrent episodes of pouchitis for several years despite several courses of antibiotic therapy. He reports at least three episodes of pouchitis in a year. The patient had multiple surveillance colonoscopies, which revealed evidence of mild chronic inflammation of the pouch. Magnetic resonance imaging (MRI) of the perineum was notable for small intersphincteric fistulous tracts extending from the anal gland, which had to be repaired. C-reactive protein (CRP) and calprotectin levels were normal. Immunoglobulin g4 (IgG4) and antineutrophil cytoplasmic antibodies were negative. Most recent biopsies taken from the pouch demonstrate moderate chronic inflammation (figure 1). Magnetic resonance cholangiopancreatography (MRCP) is negative for primary sclerosing cholangitis. The patient is being managed with mesalamine and probiotics and is currently asymptomatic.
Discussion: CARP is emerging as an entity associated with poor quality of life and increased health care costs. Genetic predisposition to immune system dysregulation is considered a contributing factor. CARP fails to respond to multiple courses of antibiotic therapy. Therefore, the management of CARP is difficult and limited. Current literature on the management of CARP is scarce and mainly involves immunomodulatory therapy and probiotics. It is essential to keep this differential diagnosis in mind in patients with recurrent pouchitis episodes and start them on immunomodulator treatment and probiotics rather than repeated courses of antibiotics.

Figure: Figure 1: A, B Histopathology showing edema, acute and chronic inflammation in the ileal villi
C. Colonscopy image demonstrating gross inflammation of the colonic mucosa
C. Colonscopy image demonstrating gross inflammation of the colonic mucosa
Disclosures:
Aditya Chauhan indicated no relevant financial relationships.
Vijay Gayam indicated no relevant financial relationships.
Praneeth Bandaru indicated no relevant financial relationships.
Srilaxmi Gujjula indicated no relevant financial relationships.
Erika Vigandt indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Denzil Etienne indicated no relevant financial relationships.
Kimberly Geckle indicated no relevant financial relationships.
Heidi Budke indicated no relevant financial relationships.
Vinaya Gaduputi indicated no relevant financial relationships.
Aditya Chauhan, MD1, Vijay Gayam, MD1, Praneeth Bandaru, MD1, Srilaxmi Gujjula, MD1, Erika Vigandt, MD1, Vikash Kumar, MD1, Denzil Etienne, MD1, Kimberly Geckle, APRN-CNP2, Heidi Budke, MD2, Vinaya Gaduputi, MD, FACG2. C0163 - Chronic Antibiotic-Resistant Pouchitis: A Complicated Entity, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
