Back
Poster Session E - Tuesday Afternoon
Category: GI Bleeding
E0307 - Early Feeding vs Delayed Feeding After Therapeutic Endoscopic Intervention in Upper GI Bleeding: A Systematic Review and Meta-Analysis
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
- WS
Wasef Sayeh, MD
University of Toledo
Toledo, Ohio
Presenting Author(s)
Award: Presidential Poster Award
Wasef Sayeh, MD1, Azizullah A. Beran, MD2, Sami Ghazaleh, MD1, Amna Iqbal, MD1, Mohammad Safi, MD1, Waleed Khokher, MD3, Bryanna Jay, MD1, Sabeen Sidiki, MD1, Rami Musallam, MD4, Ziad Abuhelwa, MD2, Sara Stanley, DO1, Ajit Ramadagu, MD3, Ali Nawras, MD1
1University of Toledo, Toledo, OH; 2The University of Toledo, Toledo, OH; 3University of Toledo Medical Center, Toledo, OH; 4St. Vincent Charity Medical Center, Cleveland, OH
Introduction: Multiple endoscopic interventions are used to treat upper GI bleeding. Early feeding after endoscopic intervention in upper GI bleeding was always thought to be associated with higher mortality rate and worse outcomes. Recent studies have investigated the role of early post procedural feeding after endoscopic interventions in patients with upper GI bleeding.
Methods: We performed a comprehensive search in the databases of PubMed/MEDLINE, Embase, and the Cochrane Central Register of Controlled Trials from inception through May 25th, 2022. We considered randomized controlled trials. We excluded abstracts, animal studies, case reports, reviews, editorials, and letters to editors. From each study, we collected the number of patients with upper GI bleeding who were started early on regular diet after the endoscopic intervention and the number of patients with delayed feeding. The primary outcome was the mortality rate. The secondary outcomes were the occurrence of early bleeding (within 7 days), late bleeding (after 7 days) and the length of hospital stay. The random-effects model was used to calculate the risk ratios (RR), mean differences (MD), and confidence intervals (CI). A p value < 0.05 was considered statistically significant. Heterogeneity was assessed using the Higgins I2 index.
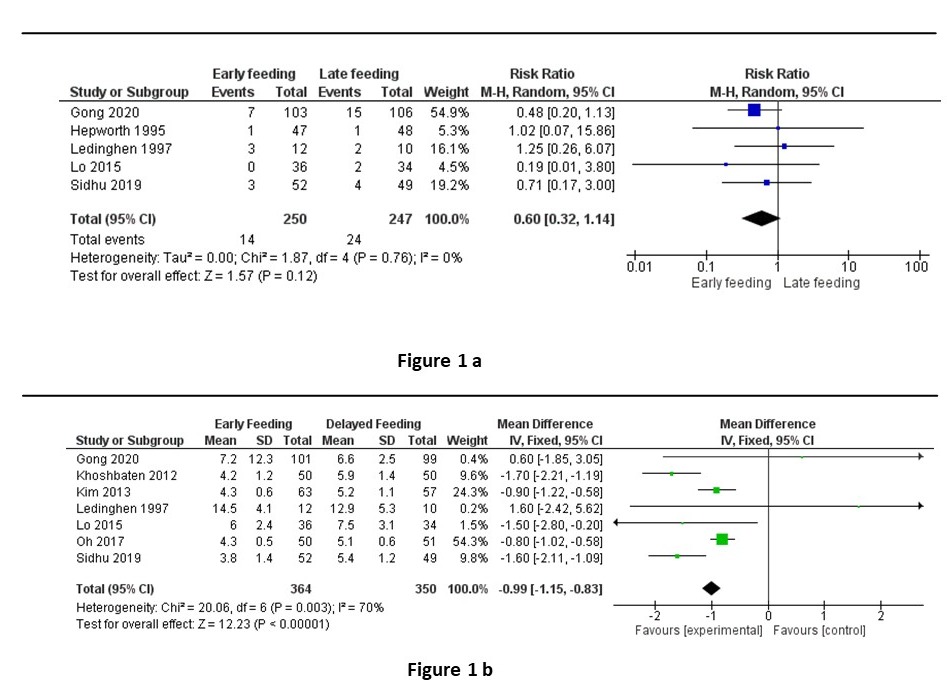
Results: Eight randomized controlled trials involving 818 patients were included in the meta-analysis. The mortality rate was not statistically different between the early feeding and the delayed feeding groups (RR 0.60, 95% CI 0.32-1.14, p =0.12, I2 = 0%) (Figure 1a). Also, the rates of both early and late bleeding were not statistically different between the two groups (RR 1.17, 95% CI 0.60-2.26, p =0.64, I2 = 0%) and (RR 0.74, 95% CI 0.25-2.14, p =0.58, I2 = 17%), respectively. However, the length of hospital stay was significantly shorter in the early feeding group (MD -0.99 days, 95% CI -1.15- -0.83, p < 0.00001, I2 = 70%) (Figure 1b).
Discussion: Our meta-analysis demonstrated that early feeding after endoscopic interventions in patients with upper GI bleeding appears to be relatively safe. There was no statistical difference in mortality rates and in early or late bleeding rates. Moreover, it was associated with a shorter hospital stay. Further randomized controlled trials are needed to confirm our findings.
Disclosures:
Wasef Sayeh, MD1, Azizullah A. Beran, MD2, Sami Ghazaleh, MD1, Amna Iqbal, MD1, Mohammad Safi, MD1, Waleed Khokher, MD3, Bryanna Jay, MD1, Sabeen Sidiki, MD1, Rami Musallam, MD4, Ziad Abuhelwa, MD2, Sara Stanley, DO1, Ajit Ramadagu, MD3, Ali Nawras, MD1. E0307 - Early Feeding vs Delayed Feeding After Therapeutic Endoscopic Intervention in Upper GI Bleeding: A Systematic Review and Meta-Analysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Wasef Sayeh, MD1, Azizullah A. Beran, MD2, Sami Ghazaleh, MD1, Amna Iqbal, MD1, Mohammad Safi, MD1, Waleed Khokher, MD3, Bryanna Jay, MD1, Sabeen Sidiki, MD1, Rami Musallam, MD4, Ziad Abuhelwa, MD2, Sara Stanley, DO1, Ajit Ramadagu, MD3, Ali Nawras, MD1
1University of Toledo, Toledo, OH; 2The University of Toledo, Toledo, OH; 3University of Toledo Medical Center, Toledo, OH; 4St. Vincent Charity Medical Center, Cleveland, OH
Introduction: Multiple endoscopic interventions are used to treat upper GI bleeding. Early feeding after endoscopic intervention in upper GI bleeding was always thought to be associated with higher mortality rate and worse outcomes. Recent studies have investigated the role of early post procedural feeding after endoscopic interventions in patients with upper GI bleeding.
Methods: We performed a comprehensive search in the databases of PubMed/MEDLINE, Embase, and the Cochrane Central Register of Controlled Trials from inception through May 25th, 2022. We considered randomized controlled trials. We excluded abstracts, animal studies, case reports, reviews, editorials, and letters to editors. From each study, we collected the number of patients with upper GI bleeding who were started early on regular diet after the endoscopic intervention and the number of patients with delayed feeding. The primary outcome was the mortality rate. The secondary outcomes were the occurrence of early bleeding (within 7 days), late bleeding (after 7 days) and the length of hospital stay. The random-effects model was used to calculate the risk ratios (RR), mean differences (MD), and confidence intervals (CI). A p value < 0.05 was considered statistically significant. Heterogeneity was assessed using the Higgins I2 index.
Results: Eight randomized controlled trials involving 818 patients were included in the meta-analysis. The mortality rate was not statistically different between the early feeding and the delayed feeding groups (RR 0.60, 95% CI 0.32-1.14, p =0.12, I2 = 0%) (Figure 1a). Also, the rates of both early and late bleeding were not statistically different between the two groups (RR 1.17, 95% CI 0.60-2.26, p =0.64, I2 = 0%) and (RR 0.74, 95% CI 0.25-2.14, p =0.58, I2 = 17%), respectively. However, the length of hospital stay was significantly shorter in the early feeding group (MD -0.99 days, 95% CI -1.15- -0.83, p < 0.00001, I2 = 70%) (Figure 1b).
Discussion: Our meta-analysis demonstrated that early feeding after endoscopic interventions in patients with upper GI bleeding appears to be relatively safe. There was no statistical difference in mortality rates and in early or late bleeding rates. Moreover, it was associated with a shorter hospital stay. Further randomized controlled trials are needed to confirm our findings.
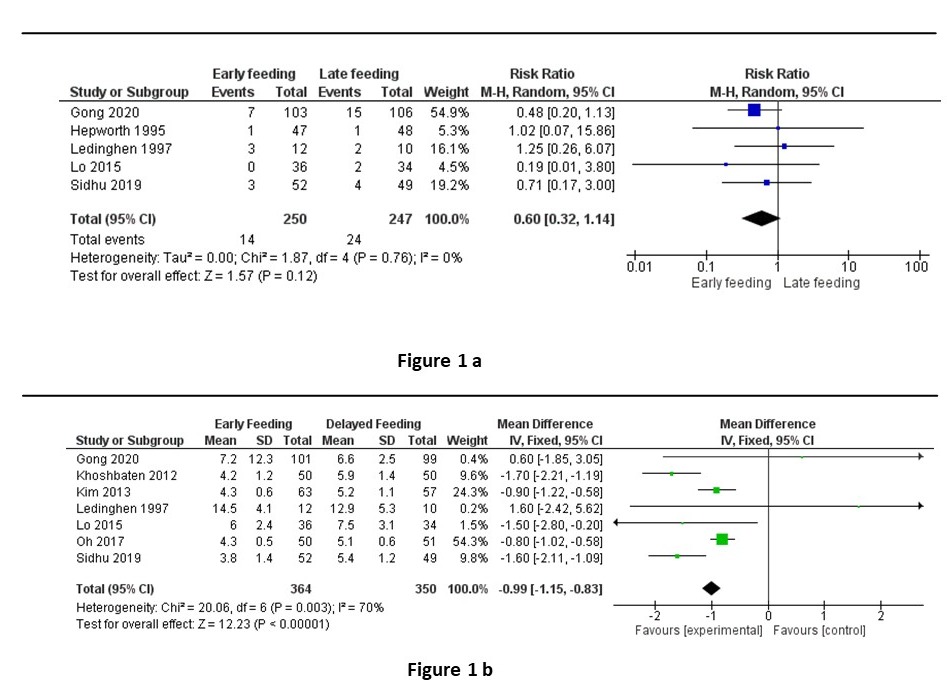
Figure: Figure 1: a) mortality rate b) the duration of hospital stay
Disclosures:
Wasef Sayeh indicated no relevant financial relationships.
Azizullah Beran indicated no relevant financial relationships.
Sami Ghazaleh indicated no relevant financial relationships.
Amna Iqbal indicated no relevant financial relationships.
Mohammad Safi indicated no relevant financial relationships.
Waleed Khokher indicated no relevant financial relationships.
Bryanna Jay indicated no relevant financial relationships.
Sabeen Sidiki indicated no relevant financial relationships.
Rami Musallam indicated no relevant financial relationships.
Ziad Abuhelwa indicated no relevant financial relationships.
Sara Stanley indicated no relevant financial relationships.
Ajit Ramadagu indicated no relevant financial relationships.
Ali Nawras indicated no relevant financial relationships.
Wasef Sayeh, MD1, Azizullah A. Beran, MD2, Sami Ghazaleh, MD1, Amna Iqbal, MD1, Mohammad Safi, MD1, Waleed Khokher, MD3, Bryanna Jay, MD1, Sabeen Sidiki, MD1, Rami Musallam, MD4, Ziad Abuhelwa, MD2, Sara Stanley, DO1, Ajit Ramadagu, MD3, Ali Nawras, MD1. E0307 - Early Feeding vs Delayed Feeding After Therapeutic Endoscopic Intervention in Upper GI Bleeding: A Systematic Review and Meta-Analysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

