Back
Poster Session E - Tuesday Afternoon
Category: GI Bleeding
E0311 - Gastric Variceal Bleed Secondary to Acute Portal Vein Thrombosis and Chronic Splenic Vein Thrombosis in the Setting of Paroxysmal Nocturnal Hematuria
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Bandhul Hans, MD
Allegheny General Hospital
Pittsburgh, Pennsylvania
Presenting Author(s)
Award: Presidential Poster Award
Bandhul Hans, MD1, Oluwakemi Adewuyi, MD2, Pamela Kim, MD1, Hui-Wei Chen, MD1
1Allegheny General Hospital, Pittsburgh, PA; 2Allegheny Health Network, Pittsburgh, PA
Introduction: PNH causes thrombosis. Long standing thrombosis causes cavernous transformation(formation of venous channels within or around a thrombosed vein).We present a case of acute gastric variceal bleeding due to extensive portal and splenic vein thrombosis from PNH
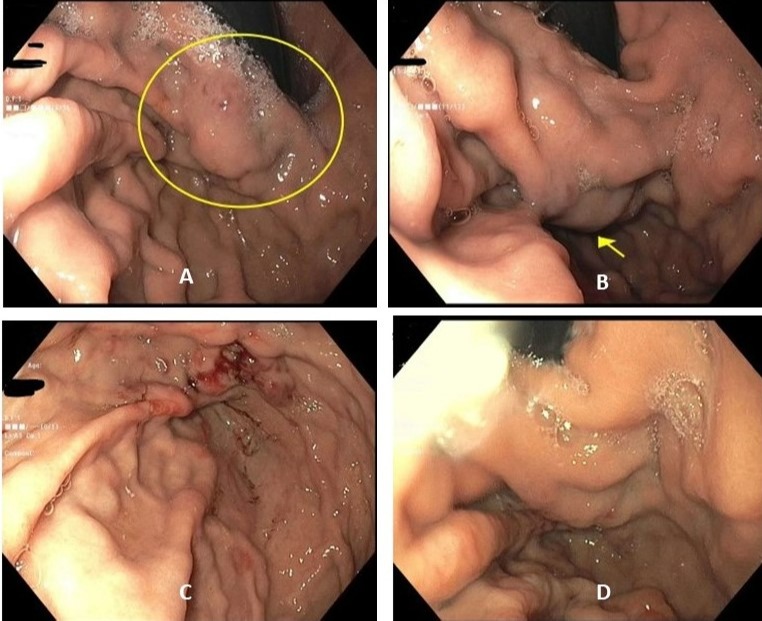
Case Description/Methods: 63/F with history of PNH presented with acute melena. CECT abdomen showed an acute, extensive,near occlusive portal vein thrombus (PVT) extending into portal vein branches and SMV with chronic occlusive splenic vein thrombus with multiple perisplenic varices. Prior CT abdomen without contrast showed splenomegaly with possible esophageal varices and pancreatic head soft tissue prominence, and an outpatient EGD/EUS done 4 days before presentation ruled out varices or pancreatic mass. She was stared on octreotide infusion and EGD showed non bleeding isolated gastric varix type 1 (IGV-1) with red wale sign (Fig A&B). Varices were thought to be secondary to extensive acute portal vein thrombosis, so she underwent IR guided mechanical thrombectomy followed by catheter directed tPA infusion with significant reduction in thrombus load. Bleeding resolved and she was discharged on anticoagulation and eculizumab for PNH. She presented 5 days later with melena and EGD showed bleeding IGV-1 not amenable to endoscopic therapy (Fig C). CT angiogram showed persistent main and left PVT with a thrombosed splenic vein with multiple collateral vessels. It was thought that the IGV-1 is secondary to focal central splenic vein occlusion and hence IR guided splenic vein recanalization with splenic varix embolization was planned but could not be attempted due to cavernous transformation of the splenic vein. Patient ultimately underwent partial embolization of the lower pole of splenic artery branches. Repeat EGD showed reduced yet present IGV -1 (Fig D) causing a rebleed 2 months later requiring her to undergo complete IR splenic artery embolization with resolution of bleeding
Discussion: While there are a few reports of cavernous transformation of portal vein (CTPV), but none with cavernous transformation of splenic vein. There is no treatment option for cavernous transformation, but complications from portal hypertension can be treated via venous thrombolysis and recanalization or arterial embolization to reduce flow with subsequent reduction and/or resolution of varices. Anticomplement therapy, eculizumab, is the only proven therapy to prevent thrombotic complication in PNH while role of prophylactic anticoagulation remains controversial
Disclosures:
Bandhul Hans, MD1, Oluwakemi Adewuyi, MD2, Pamela Kim, MD1, Hui-Wei Chen, MD1. E0311 - Gastric Variceal Bleed Secondary to Acute Portal Vein Thrombosis and Chronic Splenic Vein Thrombosis in the Setting of Paroxysmal Nocturnal Hematuria, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Bandhul Hans, MD1, Oluwakemi Adewuyi, MD2, Pamela Kim, MD1, Hui-Wei Chen, MD1
1Allegheny General Hospital, Pittsburgh, PA; 2Allegheny Health Network, Pittsburgh, PA
Introduction: PNH causes thrombosis. Long standing thrombosis causes cavernous transformation(formation of venous channels within or around a thrombosed vein).We present a case of acute gastric variceal bleeding due to extensive portal and splenic vein thrombosis from PNH
Case Description/Methods: 63/F with history of PNH presented with acute melena. CECT abdomen showed an acute, extensive,near occlusive portal vein thrombus (PVT) extending into portal vein branches and SMV with chronic occlusive splenic vein thrombus with multiple perisplenic varices. Prior CT abdomen without contrast showed splenomegaly with possible esophageal varices and pancreatic head soft tissue prominence, and an outpatient EGD/EUS done 4 days before presentation ruled out varices or pancreatic mass. She was stared on octreotide infusion and EGD showed non bleeding isolated gastric varix type 1 (IGV-1) with red wale sign (Fig A&B). Varices were thought to be secondary to extensive acute portal vein thrombosis, so she underwent IR guided mechanical thrombectomy followed by catheter directed tPA infusion with significant reduction in thrombus load. Bleeding resolved and she was discharged on anticoagulation and eculizumab for PNH. She presented 5 days later with melena and EGD showed bleeding IGV-1 not amenable to endoscopic therapy (Fig C). CT angiogram showed persistent main and left PVT with a thrombosed splenic vein with multiple collateral vessels. It was thought that the IGV-1 is secondary to focal central splenic vein occlusion and hence IR guided splenic vein recanalization with splenic varix embolization was planned but could not be attempted due to cavernous transformation of the splenic vein. Patient ultimately underwent partial embolization of the lower pole of splenic artery branches. Repeat EGD showed reduced yet present IGV -1 (Fig D) causing a rebleed 2 months later requiring her to undergo complete IR splenic artery embolization with resolution of bleeding
Discussion: While there are a few reports of cavernous transformation of portal vein (CTPV), but none with cavernous transformation of splenic vein. There is no treatment option for cavernous transformation, but complications from portal hypertension can be treated via venous thrombolysis and recanalization or arterial embolization to reduce flow with subsequent reduction and/or resolution of varices. Anticomplement therapy, eculizumab, is the only proven therapy to prevent thrombotic complication in PNH while role of prophylactic anticoagulation remains controversial
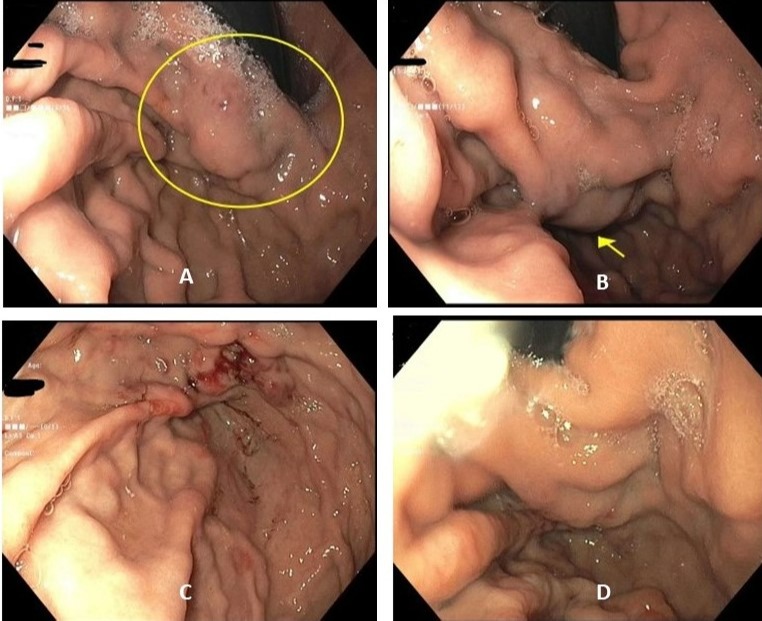
Figure: (A) & (B) Initial EGD with IGV-1 and stigmata of recent bleed. (C) Bleeding IGV-1. (D) reduction in IGV-1 after splenic artery embolization
Disclosures:
Bandhul Hans indicated no relevant financial relationships.
Oluwakemi Adewuyi indicated no relevant financial relationships.
Pamela Kim indicated no relevant financial relationships.
Hui-Wei Chen indicated no relevant financial relationships.
Bandhul Hans, MD1, Oluwakemi Adewuyi, MD2, Pamela Kim, MD1, Hui-Wei Chen, MD1. E0311 - Gastric Variceal Bleed Secondary to Acute Portal Vein Thrombosis and Chronic Splenic Vein Thrombosis in the Setting of Paroxysmal Nocturnal Hematuria, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

