Back

Poster Session E - Tuesday Afternoon
Category: GI Bleeding
E0312 - Gastro-Splenic Fistula: A Rare Cause of Upper Gastrointestinal Bleeding
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Muhammad Nadeem Yousaf, MD
University of Missouri
Columbia, MO
Presenting Author(s)
Muhammad Nadeem Yousaf, MD1, Subeena Phull, MD2, Aryal Vinayak, MD3, Karun Neupane, MD4, Hamza Ertugrul, MD1, Ebubekir Daglilar, MD1, Tahan Veysel, MD1
1University of Missouri, Columbia, MO; 2MedStar Union Memorial Hospital, Baltimore, MD; 3MetroHealth System, Case Western Reserve University, Cleveland, OH; 4Jacobi Medical Center, Albert Einstein College of Medicine, Bronx, NY
Introduction: Gastrosplenic fistula (GSF) is a rare entity. Reported etiologies of GSF are splenic or gastric malignancies, splenic abscess, Crohn’s disease, gastric ulcers, and abdominal trauma. Here, we present a case of GSF from gastric ulcer resulting in life threatening bleeding.
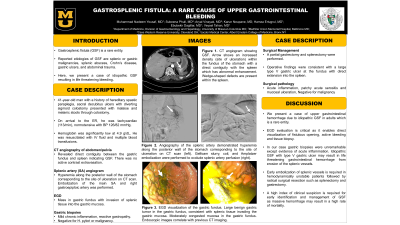
Case Description/Methods: A 41-year-old man with history of oculodentodigital dysplasia, spastic paraplegia, sacral decubitus ulcers with diverting sigmoid colostomy presented with malaise and melenic stools through colostomy. On arrival at ER, he was tachycardiac (113/min), with BP 126/82 mmHg. His Hgb was 4.9 g/dL. CT angiography of the abdomen/pelvis was negative for active contrast extravasation, however, revealed direct contiguity between the gastric fundus and spleen indicating GSF. Patient was resuscitated with IV fluid and required multiple blood transfusions. Splenic artery (SA) angiogram showed hyperemia along the posterior wall of the stomach corresponding to CT scan findings. Embolization of the main SA, right gastroepiploic, and left omental artery was performed. EGD showed benign inflammatory mass in the gastric fundus with invasion of splenic tissue into the gastric mucosa. Gastric biopsy was negative for H. pylori and malignancy, however, revealed mild chronic inflammation and reactive gastropathy. Partial gastrectomy and splenectomy were performed. Operative findings were consistent with a large type V gastric ulcer at the fundus with direct extension into the spleen. He was discharged to rehab after a prolonged hospital course.
Discussion: We present a case of GSF in the setting of type V gastric ulcer which is a rare entity. Gastric biopsies were negative for malignancy, PUD, splenic abscess, or Crohn's disease indicating the idiopathic nature of GSF. Early embolization of splenic vessels is required in hemodynamically unstable patients followed by radical surgical resection such as splenectomy and gastrectomy. A high index of clinical suspicion is required for early identification and management of GSF as massive hemorrhage results in high rate of mortality.

Disclosures:
Muhammad Nadeem Yousaf, MD1, Subeena Phull, MD2, Aryal Vinayak, MD3, Karun Neupane, MD4, Hamza Ertugrul, MD1, Ebubekir Daglilar, MD1, Tahan Veysel, MD1. E0312 - Gastro-Splenic Fistula: A Rare Cause of Upper Gastrointestinal Bleeding, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Missouri, Columbia, MO; 2MedStar Union Memorial Hospital, Baltimore, MD; 3MetroHealth System, Case Western Reserve University, Cleveland, OH; 4Jacobi Medical Center, Albert Einstein College of Medicine, Bronx, NY
Introduction: Gastrosplenic fistula (GSF) is a rare entity. Reported etiologies of GSF are splenic or gastric malignancies, splenic abscess, Crohn’s disease, gastric ulcers, and abdominal trauma. Here, we present a case of GSF from gastric ulcer resulting in life threatening bleeding.
Case Description/Methods: A 41-year-old man with history of oculodentodigital dysplasia, spastic paraplegia, sacral decubitus ulcers with diverting sigmoid colostomy presented with malaise and melenic stools through colostomy. On arrival at ER, he was tachycardiac (113/min), with BP 126/82 mmHg. His Hgb was 4.9 g/dL. CT angiography of the abdomen/pelvis was negative for active contrast extravasation, however, revealed direct contiguity between the gastric fundus and spleen indicating GSF. Patient was resuscitated with IV fluid and required multiple blood transfusions. Splenic artery (SA) angiogram showed hyperemia along the posterior wall of the stomach corresponding to CT scan findings. Embolization of the main SA, right gastroepiploic, and left omental artery was performed. EGD showed benign inflammatory mass in the gastric fundus with invasion of splenic tissue into the gastric mucosa. Gastric biopsy was negative for H. pylori and malignancy, however, revealed mild chronic inflammation and reactive gastropathy. Partial gastrectomy and splenectomy were performed. Operative findings were consistent with a large type V gastric ulcer at the fundus with direct extension into the spleen. He was discharged to rehab after a prolonged hospital course.
Discussion: We present a case of GSF in the setting of type V gastric ulcer which is a rare entity. Gastric biopsies were negative for malignancy, PUD, splenic abscess, or Crohn's disease indicating the idiopathic nature of GSF. Early embolization of splenic vessels is required in hemodynamically unstable patients followed by radical surgical resection such as splenectomy and gastrectomy. A high index of clinical suspicion is required for early identification and management of GSF as massive hemorrhage results in high rate of mortality.

Figure: CT angiogram (A) shows wedge shaped defect between gastric fundus and spleen indicating gastrosplenic fistula (arrow). Angiography of the splenic artery (B) shows extravasation of blood along the posterior wall of the stomach corresponding to the site of ulceration on the CT scan. Splenic artery angiogram after Gelfoam slurry, coil, and Amplatzer embolization (C). CT abdomen/pelvis after embolization of the main SA, right gastroepiploic, and left omental artery (D). EGD shows a large benign gastric tumor in the gastric fundus, consistent with splenic tissue invading the gastric mucosa (E-F).
Disclosures:
Muhammad Nadeem Yousaf indicated no relevant financial relationships.
Subeena Phull indicated no relevant financial relationships.
Aryal Vinayak indicated no relevant financial relationships.
Karun Neupane indicated no relevant financial relationships.
Hamza Ertugrul indicated no relevant financial relationships.
Ebubekir Daglilar indicated no relevant financial relationships.
Tahan Veysel — NO DISCLOSURE DATA.
Tahan Veysel indicated no relevant financial relationships.
Muhammad Nadeem Yousaf, MD1, Subeena Phull, MD2, Aryal Vinayak, MD3, Karun Neupane, MD4, Hamza Ertugrul, MD1, Ebubekir Daglilar, MD1, Tahan Veysel, MD1. E0312 - Gastro-Splenic Fistula: A Rare Cause of Upper Gastrointestinal Bleeding, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
