Back

Poster Session E - Tuesday Afternoon
Category: GI Bleeding
E0319 - Rare Gastrointestinal Bleeding in a Patient With Severe Plasmodium Falciparum Malaria
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Karolina Krawczyk, MD, MS
Loyola University Medical Center
Maywood , IL
Presenting Author(s)
Karolina Krawczyk, MD, MS, Jasleen Sandhu, MD, Jake Jasurda, DO, Ayokunle T. Abegunde, MD, MSc, MRCGP
Loyola University Medical Center, Maywood, IL
Introduction: Malaria clinically presents as a systemic febrile illness; the most severe form is caused by Plasmodium Falciparum. In addition to hematologic manifestations such as severe anemia, thrombocytopenia, and coagulopathy, malaria patients uncommonly experience gastrointestinal complications such as GI bleeds, splenic rupture and subacute intestinal obstruction. We report a severe case of P. falciparum malaria complicated by a GI bleed.
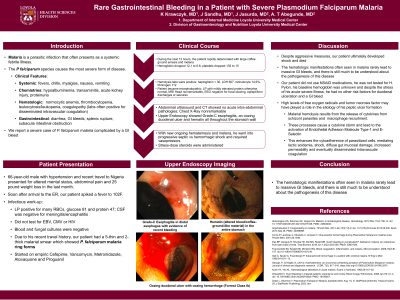
Case Description/Methods: A 66-year-old male with recent travel to Nigeria and a medical history of hypertension was brought to the ER with altered mental status, abdominal pain and a 25lb weight loss in the last month. In the ED he spiked a fever to 102F, prompting a thorough infectious workup. An LP was remarkable for many RBCs, glucose 81 and protein 47. CSF was negative for meningitis/encephalitis; he did not have EBV, CMV or HIV. Blood and fungal cultures were negative. Due to his recent travel history, our patient had a 5-thin and 2-thick malarial smear which showed P. falciparum malaria ring forms. He was started on cefepime, vancomycin, metronidazole, atovaquone/proguanil. Over the next 12-hours, the patient rapidly deteriorated with a large coffee ground emesis, a hemoglobin drop from 12.1 to 8.6, and a thrombocytopenia from 135 to 15. Hemolysis labs were positive: haptoglobin < 30, LDH 607, reticulocyte 14.6%, fibrinogen 112. Upper endoscopy showed Grade-C esophagitis, an oozing duodenal ulcer and hematin all throughout the stomach wall. Abdominal ultrasound and CT showed no acute intra-abdominal pathologies. With new ongoing hematemesis and melena, he went into progressive septic vs hemorrhagic shock and required vasopressors and stress-dose steroids.
Discussion: The hematologic manifestations often seen in malaria rarely lead to massive GI bleeds. Our patient did not use NSAIDS, he was not tested for H. Pylori, and despite the stress of his acute severe illness, he had no other risk factors for duodenal ulceration. High levels of free oxygen radicals and tumor necrosis factor may have played a role in the etiology of his peptic ulcer formation. Malarial hemolysis results from the release of cytokines, macrophage recruitment, causing a cytokine storm and activation of endothelial adhesion molecule type 1, E-selectin, enhancing cytoadherence of parasitized cells, mediating lactic acidemia, shock, gut mucosal damage and increased permeability. Despite aggressive measures, our patient ultimately developed shock and died.
Disclosures:
Karolina Krawczyk, MD, MS, Jasleen Sandhu, MD, Jake Jasurda, DO, Ayokunle T. Abegunde, MD, MSc, MRCGP. E0319 - Rare Gastrointestinal Bleeding in a Patient With Severe Plasmodium Falciparum Malaria, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Loyola University Medical Center, Maywood, IL
Introduction: Malaria clinically presents as a systemic febrile illness; the most severe form is caused by Plasmodium Falciparum. In addition to hematologic manifestations such as severe anemia, thrombocytopenia, and coagulopathy, malaria patients uncommonly experience gastrointestinal complications such as GI bleeds, splenic rupture and subacute intestinal obstruction. We report a severe case of P. falciparum malaria complicated by a GI bleed.
Case Description/Methods: A 66-year-old male with recent travel to Nigeria and a medical history of hypertension was brought to the ER with altered mental status, abdominal pain and a 25lb weight loss in the last month. In the ED he spiked a fever to 102F, prompting a thorough infectious workup. An LP was remarkable for many RBCs, glucose 81 and protein 47. CSF was negative for meningitis/encephalitis; he did not have EBV, CMV or HIV. Blood and fungal cultures were negative. Due to his recent travel history, our patient had a 5-thin and 2-thick malarial smear which showed P. falciparum malaria ring forms. He was started on cefepime, vancomycin, metronidazole, atovaquone/proguanil. Over the next 12-hours, the patient rapidly deteriorated with a large coffee ground emesis, a hemoglobin drop from 12.1 to 8.6, and a thrombocytopenia from 135 to 15. Hemolysis labs were positive: haptoglobin < 30, LDH 607, reticulocyte 14.6%, fibrinogen 112. Upper endoscopy showed Grade-C esophagitis, an oozing duodenal ulcer and hematin all throughout the stomach wall. Abdominal ultrasound and CT showed no acute intra-abdominal pathologies. With new ongoing hematemesis and melena, he went into progressive septic vs hemorrhagic shock and required vasopressors and stress-dose steroids.
Discussion: The hematologic manifestations often seen in malaria rarely lead to massive GI bleeds. Our patient did not use NSAIDS, he was not tested for H. Pylori, and despite the stress of his acute severe illness, he had no other risk factors for duodenal ulceration. High levels of free oxygen radicals and tumor necrosis factor may have played a role in the etiology of his peptic ulcer formation. Malarial hemolysis results from the release of cytokines, macrophage recruitment, causing a cytokine storm and activation of endothelial adhesion molecule type 1, E-selectin, enhancing cytoadherence of parasitized cells, mediating lactic acidemia, shock, gut mucosal damage and increased permeability. Despite aggressive measures, our patient ultimately developed shock and died.
Disclosures:
Karolina Krawczyk indicated no relevant financial relationships.
Jasleen Sandhu indicated no relevant financial relationships.
Jake Jasurda indicated no relevant financial relationships.
Ayokunle Abegunde indicated no relevant financial relationships.
Karolina Krawczyk, MD, MS, Jasleen Sandhu, MD, Jake Jasurda, DO, Ayokunle T. Abegunde, MD, MSc, MRCGP. E0319 - Rare Gastrointestinal Bleeding in a Patient With Severe Plasmodium Falciparum Malaria, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
