Back

Poster Session C - Monday Afternoon
Category: Colon
C0161 - Posterior Solitary Rectal Ulcer Syndrome
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Joshua T. Mathews, DO
Guthrie Robert Packer Hospital
Sayre, PA
Presenting Author(s)
Joshua T. Mathews, DO1, Sudhir Pasham, MBBS1, Alexander Miller, MBBS, MD2, Matthew Lincoln, MD3
1Guthrie Robert Packer Hospital Gastroenterology Fellowship, Sayre, PA; 2Guthrie RPH, Sayre, PA; 3Guthrie Robert Packer Hospital, Sayre, PA
Introduction: Solitary rectal ulcer syndrome (SRUS) is a rare colorectal disorder that presents as bright red blood per rectum (BRBPR), rectal pain, straining, incomplete evacuation, and rectal prolapse. The incidence of SRUS is 1: 100,000 individuals per year. SRUS is a misnomer as it can present as multiple ulcers and polypoid lesions. Differential diagnoses include inflammatory bowel disease (IBD), ischemic colitis, pseudomembranous colitis, and malignancy. Ergo, histopathological evaluation is necessary for differentiation. Typically, these lesions occur on the anterior surface of the rectum given the movement of the muscles in the rectum. In our case, we present a patient who has a posterior SRUS which was misdiagnosed as Crohn’s disease.
Case Description/Methods: 45-y.o. heterosexual male with PMH of presumed Crohn’s and diverticulosis presented to ED multiple times with recurrent complaints of BRBPR & abdominal pain intermittently over 18 years. Imaging showed rectal wall thickening & inflammation. Patient underwent multiple sigmoidoscopies and colonoscopies showing a single ulcer in the posterior with stigmata of bleeding. Multiple clips and hemostatic therapies were applied. Repeat biopsy results showed chronic ulceration with reactive rectal epithelium; all negative for dysplasia/malignancy and no evidence of IBD. Patient was treated conservatively with mesalamine enemas, steroids, & laxatives. Defacogram was normal. Given repeated episodes of bleeding despite this, colorectal surgery performed a laparoscopic low anterior resection of the ulcer.
Discussion: The pathogenesis behind SRUS is poorly understood but thought to be a result of rectal prolapse and rectal trauma by 2 different mechanisms. 1) Prolapsed rectal mucosa forced downward due to the pressures generated by the rectum during defecation, while opposing forces of the paradoxical contraction of the puborectalis muscle tendon cause high pressures within the rectum, leading to mucosal ischemia, and predisposing to ulceration. 2) Contraction of the puborectalis muscle result in shear forces on the rectal mucosa. Treatment is biofeedback therapy and topical therapies. Surgery is a last resort. A postero-lateral rectal ulcer is atypical unlike the usual anterior ulcers. Our patient was noted to have an exaggerated cul-de-sac along with a partially prolapsed anterior wall of rectum. Post op, he is doing well without any clinical symptoms.
Disclosures:
Joshua T. Mathews, DO1, Sudhir Pasham, MBBS1, Alexander Miller, MBBS, MD2, Matthew Lincoln, MD3. C0161 - Posterior Solitary Rectal Ulcer Syndrome, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Guthrie Robert Packer Hospital Gastroenterology Fellowship, Sayre, PA; 2Guthrie RPH, Sayre, PA; 3Guthrie Robert Packer Hospital, Sayre, PA
Introduction: Solitary rectal ulcer syndrome (SRUS) is a rare colorectal disorder that presents as bright red blood per rectum (BRBPR), rectal pain, straining, incomplete evacuation, and rectal prolapse. The incidence of SRUS is 1: 100,000 individuals per year. SRUS is a misnomer as it can present as multiple ulcers and polypoid lesions. Differential diagnoses include inflammatory bowel disease (IBD), ischemic colitis, pseudomembranous colitis, and malignancy. Ergo, histopathological evaluation is necessary for differentiation. Typically, these lesions occur on the anterior surface of the rectum given the movement of the muscles in the rectum. In our case, we present a patient who has a posterior SRUS which was misdiagnosed as Crohn’s disease.
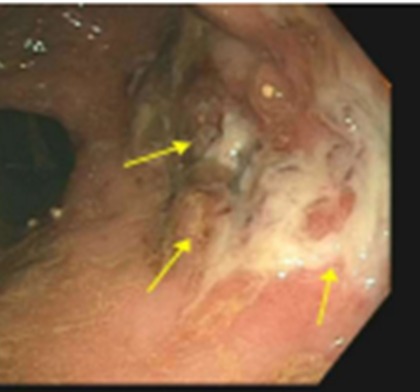
Case Description/Methods: 45-y.o. heterosexual male with PMH of presumed Crohn’s and diverticulosis presented to ED multiple times with recurrent complaints of BRBPR & abdominal pain intermittently over 18 years. Imaging showed rectal wall thickening & inflammation. Patient underwent multiple sigmoidoscopies and colonoscopies showing a single ulcer in the posterior with stigmata of bleeding. Multiple clips and hemostatic therapies were applied. Repeat biopsy results showed chronic ulceration with reactive rectal epithelium; all negative for dysplasia/malignancy and no evidence of IBD. Patient was treated conservatively with mesalamine enemas, steroids, & laxatives. Defacogram was normal. Given repeated episodes of bleeding despite this, colorectal surgery performed a laparoscopic low anterior resection of the ulcer.
Discussion: The pathogenesis behind SRUS is poorly understood but thought to be a result of rectal prolapse and rectal trauma by 2 different mechanisms. 1) Prolapsed rectal mucosa forced downward due to the pressures generated by the rectum during defecation, while opposing forces of the paradoxical contraction of the puborectalis muscle tendon cause high pressures within the rectum, leading to mucosal ischemia, and predisposing to ulceration. 2) Contraction of the puborectalis muscle result in shear forces on the rectal mucosa. Treatment is biofeedback therapy and topical therapies. Surgery is a last resort. A postero-lateral rectal ulcer is atypical unlike the usual anterior ulcers. Our patient was noted to have an exaggerated cul-de-sac along with a partially prolapsed anterior wall of rectum. Post op, he is doing well without any clinical symptoms.
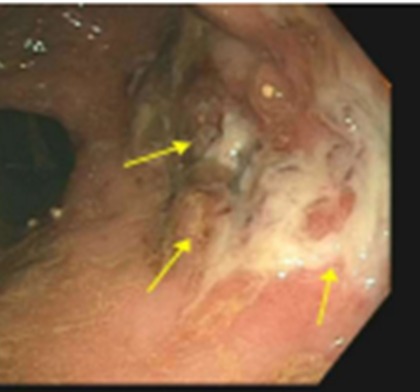
Figure: Posterior SRUS
Disclosures:
Joshua Mathews indicated no relevant financial relationships.
Sudhir Pasham indicated no relevant financial relationships.
Alexander Miller indicated no relevant financial relationships.
Matthew Lincoln indicated no relevant financial relationships.
Joshua T. Mathews, DO1, Sudhir Pasham, MBBS1, Alexander Miller, MBBS, MD2, Matthew Lincoln, MD3. C0161 - Posterior Solitary Rectal Ulcer Syndrome, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
