Back

Poster Session E - Tuesday Afternoon
Category: GI Bleeding
E0340 - Severe Lupus Enteritis Complicated by Intractable Gastrointestinal Hemorrhage
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Austin R. Thomas, DO
University of Texas Health Science Center
Houston, TX
Presenting Author(s)
Austin R. Thomas, DO1, Athira Jayan, MD2, Maneera Chopra, MD3, Faisal Ali, MD1, Karim Doughem, MD4, Joanna Scoon, MD5, Scott Larson, MD, PhD6
1University of Texas Health Science Center, Houston, TX; 2UT Houston Health Science Center, Houston, TX; 3The University of Texas Health Science Center at Houston, Houston, TX; 4University of Texas - McGovern Medical School, Houston, TX; 5University of Texas at Houston McGovern Medical School, Houston, TX; 6UT Houston McGovern Medical School, Houston, TX
Introduction: Lupus enteritis (LE) is a rare presentation of systemic lupus erythematosus (SLE) which can manifest as gastrointestinal (GI) hemorrhage, bowel perforation, and even death. Endoscopic intervention, though often performed, rarely leads to control of disease and may carry a risk of considerable harm. Immunosuppression remains the cornerstone for the treatment of the underlying disease process. Herein, we demonstrate the utility of endoscopy and immunosuppression in a patient with LE.
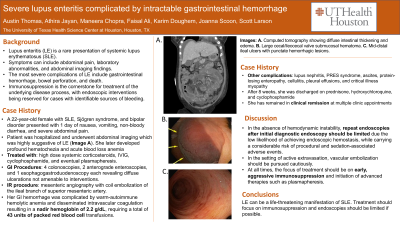
Case Description/Methods: A 22-year-old female with SLE, Sjögren syndrome, and bipolar disorder presented to a tertiary care center with one day of nausea, vomiting, non-bloody diarrhea, and severe abdominal pain. The patient was hospitalized and computed tomography revealed findings suggestive of LE. Over the course of her hospital stay, she developed profound hematochezia requiring massive transfusions on multiple occasions. The GI service was consulted for assistance with severe bleeding from LE; she underwent a total of 4 colonoscopies, 2 anterograde enteroscopies, and 1 esophagogastroduodenoscopy; all revealed diffuse ulcerations and oozing lesions that could not be treated endoscopically. She also underwent mesenteric angiography with coil embolization of the ileal branch of the superior mesenteric artery which had active extravasation into the GI tract. However, this did not curb the severity of her bleeding. Her GI hemorrhage was complicated by warm-autoimmune hemolytic anemia and disseminated intravascular coagulation resulting in a nadir hemoglobin of 2.2 g/dL despite receiving high dose systemic corticosteroids and cyclophosphamide. She required a total of 43 units of packed red blood cell transfusions. The patient eventually achieved adequate clinical response after 3 days of intravenous immunoglobulin infusion and 5 cycles of plasmapheresis.
Discussion: GI hemorrhage in the setting of immune-mediated enteritis and colitis should be managed with aggressive immunosuppression. In the absence of hemodynamic instability, repeat endoscopies after initial diagnostic endoscopy should be limited due to the low likelihood of achieving endoscopic hemostasis, while carrying a considerable risk of procedural and sedation-associated adverse events. In the setting of active extravasation, vascular embolization should be pursued cautiously. At all times, the focus of treatment should be on early, aggressive immunosuppression and the initiation of advanced therapies such as plasmapheresis.
Disclosures:
Austin R. Thomas, DO1, Athira Jayan, MD2, Maneera Chopra, MD3, Faisal Ali, MD1, Karim Doughem, MD4, Joanna Scoon, MD5, Scott Larson, MD, PhD6. E0340 - Severe Lupus Enteritis Complicated by Intractable Gastrointestinal Hemorrhage, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Texas Health Science Center, Houston, TX; 2UT Houston Health Science Center, Houston, TX; 3The University of Texas Health Science Center at Houston, Houston, TX; 4University of Texas - McGovern Medical School, Houston, TX; 5University of Texas at Houston McGovern Medical School, Houston, TX; 6UT Houston McGovern Medical School, Houston, TX
Introduction: Lupus enteritis (LE) is a rare presentation of systemic lupus erythematosus (SLE) which can manifest as gastrointestinal (GI) hemorrhage, bowel perforation, and even death. Endoscopic intervention, though often performed, rarely leads to control of disease and may carry a risk of considerable harm. Immunosuppression remains the cornerstone for the treatment of the underlying disease process. Herein, we demonstrate the utility of endoscopy and immunosuppression in a patient with LE.
Case Description/Methods: A 22-year-old female with SLE, Sjögren syndrome, and bipolar disorder presented to a tertiary care center with one day of nausea, vomiting, non-bloody diarrhea, and severe abdominal pain. The patient was hospitalized and computed tomography revealed findings suggestive of LE. Over the course of her hospital stay, she developed profound hematochezia requiring massive transfusions on multiple occasions. The GI service was consulted for assistance with severe bleeding from LE; she underwent a total of 4 colonoscopies, 2 anterograde enteroscopies, and 1 esophagogastroduodenoscopy; all revealed diffuse ulcerations and oozing lesions that could not be treated endoscopically. She also underwent mesenteric angiography with coil embolization of the ileal branch of the superior mesenteric artery which had active extravasation into the GI tract. However, this did not curb the severity of her bleeding. Her GI hemorrhage was complicated by warm-autoimmune hemolytic anemia and disseminated intravascular coagulation resulting in a nadir hemoglobin of 2.2 g/dL despite receiving high dose systemic corticosteroids and cyclophosphamide. She required a total of 43 units of packed red blood cell transfusions. The patient eventually achieved adequate clinical response after 3 days of intravenous immunoglobulin infusion and 5 cycles of plasmapheresis.
Discussion: GI hemorrhage in the setting of immune-mediated enteritis and colitis should be managed with aggressive immunosuppression. In the absence of hemodynamic instability, repeat endoscopies after initial diagnostic endoscopy should be limited due to the low likelihood of achieving endoscopic hemostasis, while carrying a considerable risk of procedural and sedation-associated adverse events. In the setting of active extravasation, vascular embolization should be pursued cautiously. At all times, the focus of treatment should be on early, aggressive immunosuppression and the initiation of advanced therapies such as plasmapheresis.
Disclosures:
Austin Thomas indicated no relevant financial relationships.
Athira Jayan indicated no relevant financial relationships.
Maneera Chopra indicated no relevant financial relationships.
Faisal Ali indicated no relevant financial relationships.
Karim Doughem indicated no relevant financial relationships.
Joanna Scoon indicated no relevant financial relationships.
Scott Larson: Motus GI – Consultant.
Austin R. Thomas, DO1, Athira Jayan, MD2, Maneera Chopra, MD3, Faisal Ali, MD1, Karim Doughem, MD4, Joanna Scoon, MD5, Scott Larson, MD, PhD6. E0340 - Severe Lupus Enteritis Complicated by Intractable Gastrointestinal Hemorrhage, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

