Back

Poster Session D - Tuesday Morning
Category: Biliary/Pancreas
D0083 - A Disappearing Act: Spontaneously Resolving Pancreatic Pseudocyst Mimicking Duodenal Neoplasm
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
Jay Kanaparthi, MD
Temple University Hospital
Philadelphia, PA
Presenting Author(s)
Jay Kanaparthi, MD1, Neil Mehta, MD1, Aatif Khurshid, MD1, Kamal Baig, MD1, Saraswathi Cappelle, DO2
1Temple University Hospital, Philadelphia, PA; 2Lewis Katz School of Medicine at Temple University, Philadelphia, PA
Introduction: Pancreatic head lesions have a broad differential ranging from inflammatory to malignant etiologies. Here we present a case of a pancreatic pseudocyst with surrounding inflammation mimicking a duodenal mass with neoplastic appearance on EGD/EUS only to spontaneously resolve weeks later.
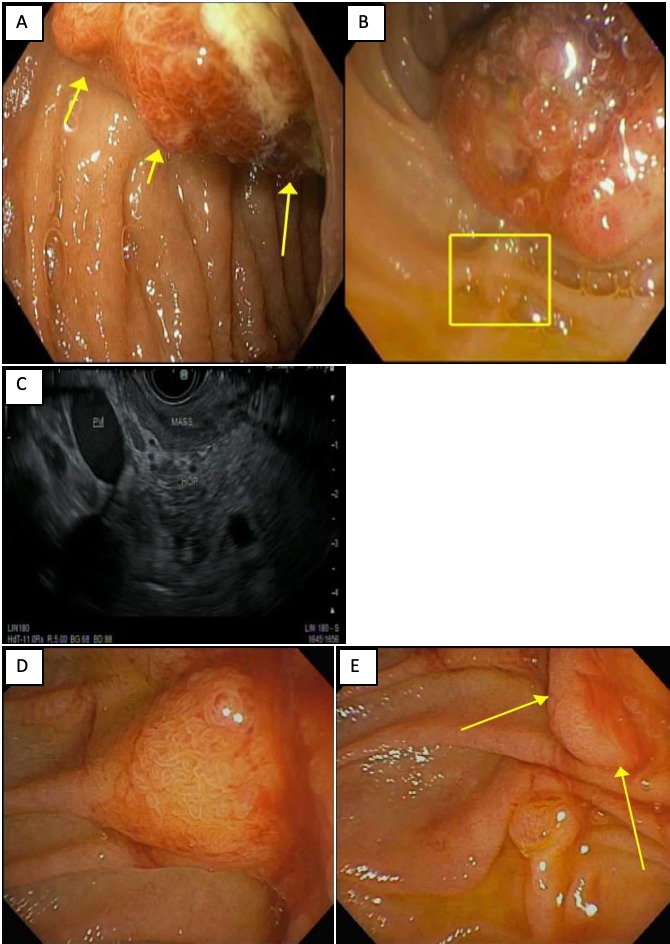
Case Description/Methods: A 49-year-old female with history of decompensated liver cirrhosis secondary to alcohol use presented with persistent nausea, vomiting, abdominal pain, and 10-pound weight loss. A CT revealed a 5.4x4.1x4.1 cm “pancreatic head mass” with heterogeneous enhancement of the right hepatic lobe and mesentery concerning for metastasis. CA 19-9, CEA, and AFP were all normal. A repeat CT with pancreatic protocol was subsequently performed suggesting the mass may be a cystic lesion with mass effect over the proximal duodenum with heterogeneous contents more consistent with a pancreatic pseudocyst. Therefore, we performed an EGD/EUS for further delineation. This procedure revealed a large ulcerated, fungating and infiltrative peri-ampullary duodenal mass at the 2nd portion of the duodenum, sparing the major papilla. On EUS, the “mass” measured 4.0x3.8 cm spanning the mucosa to the preduodenal region with close abutment to the pancreatic head. We collected biopsies of the duodenal mass and alerted the patient to her potential cancer diagnosis. She was discharged home with palliative support to follow up as an outpatient. Biopsy results returned as benign duodenal mucosa admixed with inflamed granulation tissue but no tumor. Given continued concern for a mass, a repeat CT was performed several weeks later with a shocking interval resolution of both the aforementioned pancreatic head lesion and the adjacent duodenal thickening. The next month an EGD was performed for a separate indication, in which the peri-ampullary duodenal lesion appeared smaller with significant improvement. Repeat biopsy again showed inflamed duodenal mucosa with no dysplasia. Our follow up MRI with pancreas protocol confirmed resolution of the lesion.
Discussion: With this patient’s clinical and radiological signs of cancer, further diagnostic evaluation was required with EGD/EUS. However, here we saw an unusual presentation of a duodenal “mass” on endoscopy later revealed to be a pancreatic pseudocyst with adjacent organ involvement based on diagnostic sampling and spontaneous resolution on follow up imaging. It is important to be wary of non-neoplastic processes that may mimic neoplastic ones.
Disclosures:
Jay Kanaparthi, MD1, Neil Mehta, MD1, Aatif Khurshid, MD1, Kamal Baig, MD1, Saraswathi Cappelle, DO2. D0083 - A Disappearing Act: Spontaneously Resolving Pancreatic Pseudocyst Mimicking Duodenal Neoplasm, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Temple University Hospital, Philadelphia, PA; 2Lewis Katz School of Medicine at Temple University, Philadelphia, PA
Introduction: Pancreatic head lesions have a broad differential ranging from inflammatory to malignant etiologies. Here we present a case of a pancreatic pseudocyst with surrounding inflammation mimicking a duodenal mass with neoplastic appearance on EGD/EUS only to spontaneously resolve weeks later.
Case Description/Methods: A 49-year-old female with history of decompensated liver cirrhosis secondary to alcohol use presented with persistent nausea, vomiting, abdominal pain, and 10-pound weight loss. A CT revealed a 5.4x4.1x4.1 cm “pancreatic head mass” with heterogeneous enhancement of the right hepatic lobe and mesentery concerning for metastasis. CA 19-9, CEA, and AFP were all normal. A repeat CT with pancreatic protocol was subsequently performed suggesting the mass may be a cystic lesion with mass effect over the proximal duodenum with heterogeneous contents more consistent with a pancreatic pseudocyst. Therefore, we performed an EGD/EUS for further delineation. This procedure revealed a large ulcerated, fungating and infiltrative peri-ampullary duodenal mass at the 2nd portion of the duodenum, sparing the major papilla. On EUS, the “mass” measured 4.0x3.8 cm spanning the mucosa to the preduodenal region with close abutment to the pancreatic head. We collected biopsies of the duodenal mass and alerted the patient to her potential cancer diagnosis. She was discharged home with palliative support to follow up as an outpatient. Biopsy results returned as benign duodenal mucosa admixed with inflamed granulation tissue but no tumor. Given continued concern for a mass, a repeat CT was performed several weeks later with a shocking interval resolution of both the aforementioned pancreatic head lesion and the adjacent duodenal thickening. The next month an EGD was performed for a separate indication, in which the peri-ampullary duodenal lesion appeared smaller with significant improvement. Repeat biopsy again showed inflamed duodenal mucosa with no dysplasia. Our follow up MRI with pancreas protocol confirmed resolution of the lesion.
Discussion: With this patient’s clinical and radiological signs of cancer, further diagnostic evaluation was required with EGD/EUS. However, here we saw an unusual presentation of a duodenal “mass” on endoscopy later revealed to be a pancreatic pseudocyst with adjacent organ involvement based on diagnostic sampling and spontaneous resolution on follow up imaging. It is important to be wary of non-neoplastic processes that may mimic neoplastic ones.
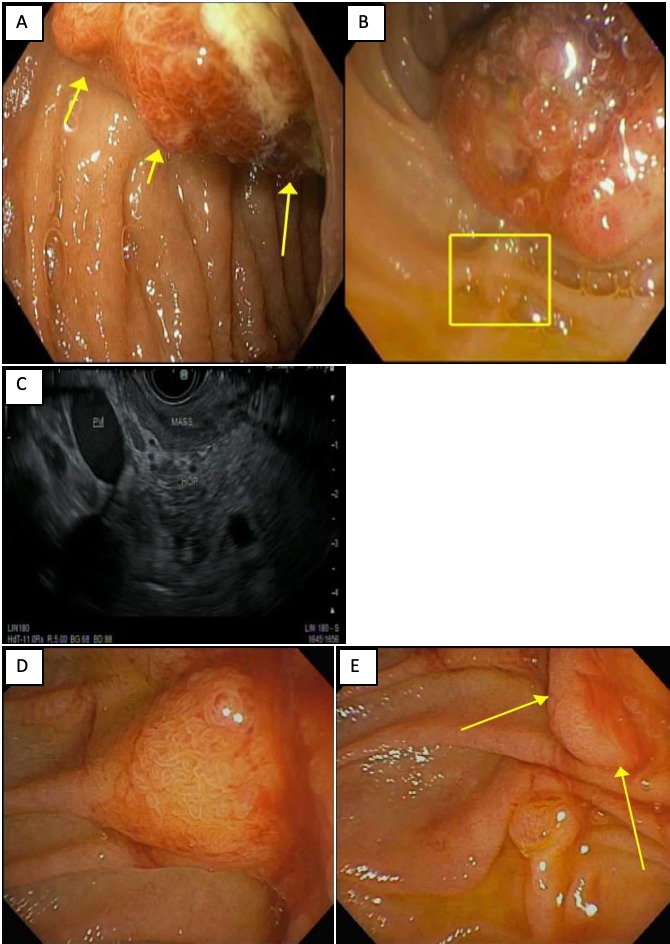
Figure: Figure 1. (A) Duodenal mass visualized from forwarding viewing scope in 2nd portion of duodenum. (B) Duodenal mass and major papilla (square) visualized with duodenoscope. (C) EUS imaging with the head of the pancreas, the duodenal mass, and portal vein. (D+E) Resolving peri-ampullary duodenal lesion on repeat EGD.
Disclosures:
Jay Kanaparthi indicated no relevant financial relationships.
Neil Mehta indicated no relevant financial relationships.
Aatif Khurshid indicated no relevant financial relationships.
Kamal Baig indicated no relevant financial relationships.
Saraswathi Cappelle: Olympus – Consultant.
Jay Kanaparthi, MD1, Neil Mehta, MD1, Aatif Khurshid, MD1, Kamal Baig, MD1, Saraswathi Cappelle, DO2. D0083 - A Disappearing Act: Spontaneously Resolving Pancreatic Pseudocyst Mimicking Duodenal Neoplasm, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
