Back

Poster Session D - Tuesday Morning
Category: Biliary/Pancreas
D0030 - A Rare Case of Extra Pulmonary Tuberculosis Involving the Pancreas and Distal Esophagus
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Omar Calderon, Jr., MD
University of South Florida
Tampa, FL
Presenting Author(s)
Omar Calderon, MD, Jonathan Hilal, MD
University of South Florida, Tampa, FL
Introduction: We report an unusual case of extra-pulmonary tuberculosis (TB) involving the esophagus and pancreas. The case presented a diagnostic challenge with unrevealing original core biopsy and a battery of infectious, inflammatory, rheumatologic, and procedural testing.
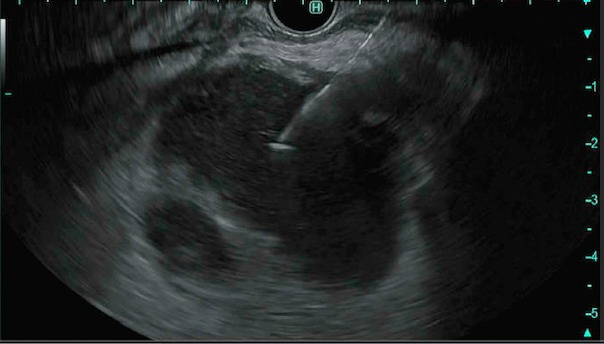
Case Description/Methods: A 54-year-old female with a past medical history of renal transplant and latent TB treated with isoniazid presented from a regional hospital for further evaluation of epigastric pain associated with 15-pound weight loss. On admission, the patient was afebrile, hemodynamically stable, with mild epigastric abdominal tenderness without rebound or guarding. Her labs were significant for mild leukocytosis, normocytic anemia, and hyponatremia. Computerized tomography of the abdomen and pelvis was remarkable for extensive retroperitoneal adenopathy, circumferential esophageal wall thickening, and a peripancreatic mass. At the transferring hospital the patient underwent a core needle biopsy of the retroperitoneal mass with pathology showing granulomatous inflammation with necrosis and no evidence of malignancy. The patient was subsequently transferred to our hospital for further evaluation. After extensive infectious and rheumatologic workup, including bronchoalveolar lavage, the patient underwent endoscopic ultrasound-fine needle aspiration, which showed an irregular 5.6 cm by 5 cm mass in the peripancreatic region with mixed features near the body and tail. A fine needle biopsy was performed, and 45 milliliters of cloudy, yellow, purulent fluid was sent for pathology and microbiology. Gastric and distal esophageal biopsies were also sent for pathology. The final report was significant for acid-fast bacilli in the esophagus and the pancreas. The fluid analysis of the pancreas with real-time polymerase chain reaction (PCR) was positive for Mycobacterium tuberculosis. The patient was subsequently treated with rifabutin, isoniazid, pyrazinamide, and ethambutol.
Discussion: Extra-pulmonary tuberculosis manifesting in the pancreas or esophagus is extraordinarily rare. Per the literature review, there are no reported synchronous pancreatic-esophageal tuberculosis cases. Esophageal tuberculosis mainly presents as an extension of pulmonary disease. Pancreatic tuberculosis generally presents as a pancreatic mass and is often misdiagnosed as a pancreatic adenocarcinoma. This case demonstrates the deceptive nature of tuberculosis and its capability to afflict the gastrointestinal system.
Disclosures:
Omar Calderon, MD, Jonathan Hilal, MD. D0030 - A Rare Case of Extra Pulmonary Tuberculosis Involving the Pancreas and Distal Esophagus, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
University of South Florida, Tampa, FL
Introduction: We report an unusual case of extra-pulmonary tuberculosis (TB) involving the esophagus and pancreas. The case presented a diagnostic challenge with unrevealing original core biopsy and a battery of infectious, inflammatory, rheumatologic, and procedural testing.
Case Description/Methods: A 54-year-old female with a past medical history of renal transplant and latent TB treated with isoniazid presented from a regional hospital for further evaluation of epigastric pain associated with 15-pound weight loss. On admission, the patient was afebrile, hemodynamically stable, with mild epigastric abdominal tenderness without rebound or guarding. Her labs were significant for mild leukocytosis, normocytic anemia, and hyponatremia. Computerized tomography of the abdomen and pelvis was remarkable for extensive retroperitoneal adenopathy, circumferential esophageal wall thickening, and a peripancreatic mass. At the transferring hospital the patient underwent a core needle biopsy of the retroperitoneal mass with pathology showing granulomatous inflammation with necrosis and no evidence of malignancy. The patient was subsequently transferred to our hospital for further evaluation. After extensive infectious and rheumatologic workup, including bronchoalveolar lavage, the patient underwent endoscopic ultrasound-fine needle aspiration, which showed an irregular 5.6 cm by 5 cm mass in the peripancreatic region with mixed features near the body and tail. A fine needle biopsy was performed, and 45 milliliters of cloudy, yellow, purulent fluid was sent for pathology and microbiology. Gastric and distal esophageal biopsies were also sent for pathology. The final report was significant for acid-fast bacilli in the esophagus and the pancreas. The fluid analysis of the pancreas with real-time polymerase chain reaction (PCR) was positive for Mycobacterium tuberculosis. The patient was subsequently treated with rifabutin, isoniazid, pyrazinamide, and ethambutol.
Discussion: Extra-pulmonary tuberculosis manifesting in the pancreas or esophagus is extraordinarily rare. Per the literature review, there are no reported synchronous pancreatic-esophageal tuberculosis cases. Esophageal tuberculosis mainly presents as an extension of pulmonary disease. Pancreatic tuberculosis generally presents as a pancreatic mass and is often misdiagnosed as a pancreatic adenocarcinoma. This case demonstrates the deceptive nature of tuberculosis and its capability to afflict the gastrointestinal system.
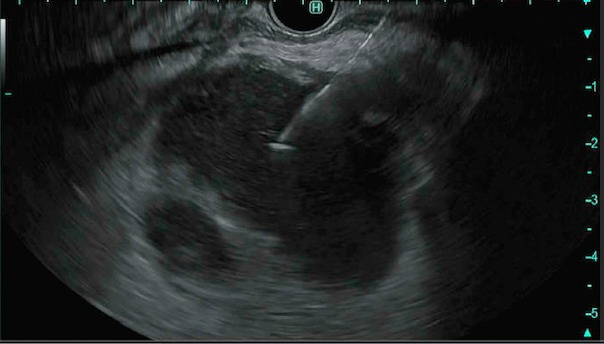
Figure: Endoscopic ultrasound-fine needle aspiration of pancreatic mass
Disclosures:
Omar Calderon indicated no relevant financial relationships.
Jonathan Hilal indicated no relevant financial relationships.
Omar Calderon, MD, Jonathan Hilal, MD. D0030 - A Rare Case of Extra Pulmonary Tuberculosis Involving the Pancreas and Distal Esophagus, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
